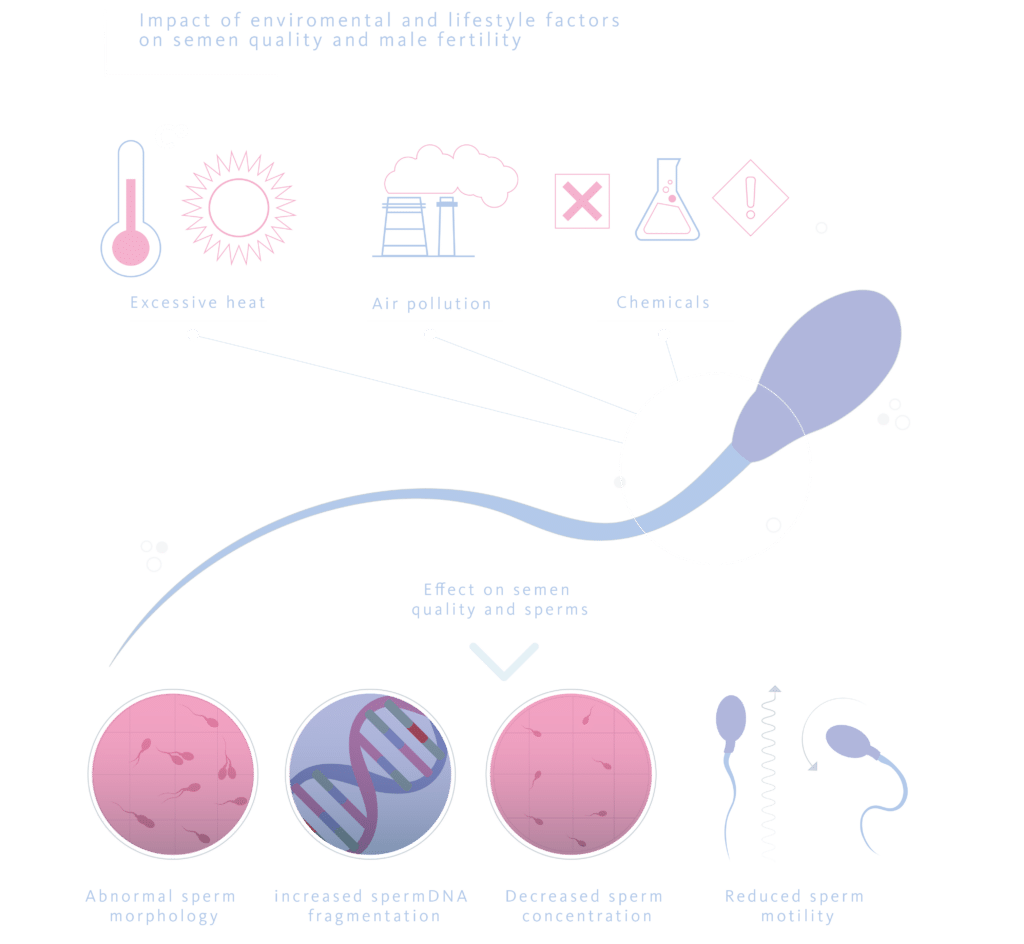
About 8-12% of couples worldwide suffer from infertility, with male factors implicated in 50% of cases. Various causes can predispose a man to infertility, including hormonal, genetic, behavioural, iatrogenic, environmental, and lifestyle factors. Given that a significant percentage of the human population is exposed to pollutants, and that the World Health Organisation considers these pollutants responsible for the deterioration of health in those who come into contact with them, the link between infertility and the presence of environmental pollutants has become increasingly important in recent years. Among other issues, environmental pollutants have been blamed for the worrying trend of declining semen quality.
What environmental factors affect the decline in sperm quality?
Numerous natural and man-made substances are released into the environment daily, which have harmful effects on male fertility. Although these adverse effects on spermatogenesis are known, we have very little data on how they act. The available studies are usually conducted in occupational settings or on people exposed to high concentrations of these substances, and there are almost no studies in the general population.
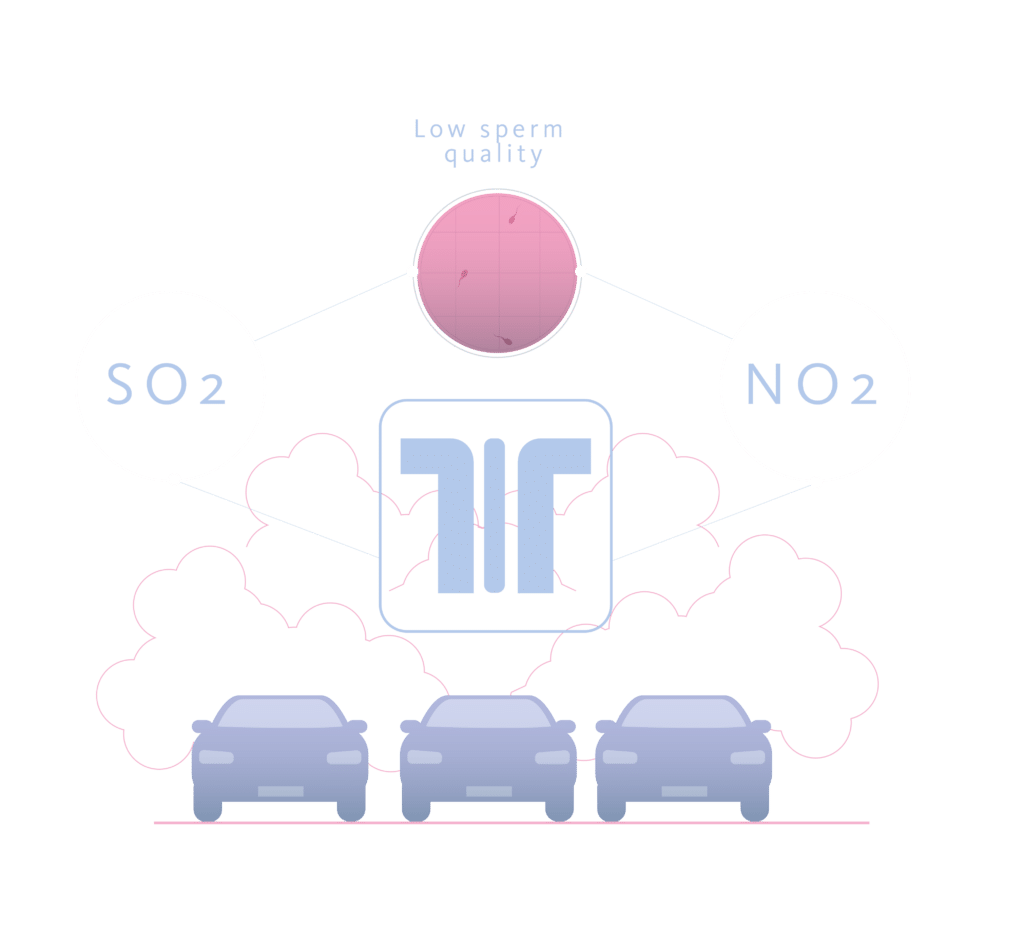
For example, one study analysed the semen quality of motorway toll workers and found that total sperm motility, progressive sperm motility, and sperm kinetics were significantly lower compared to men who lived in the area and had other occupations. From this and similar studies, it was determined that exposure to sulphur dioxide (SO2), nitrogen dioxide (NO2), and lead affects sperm parameters. On the other hand, it has been reported that ozone, another air pollutant, can decrease the percentage of spermatozoa with normal morphology.
In polluted air, solid particles measuring 2.5 microns in diameter, known as PM2.5 particles, are a significant component of haze and an indicator of air pollution. These particles can consist of various components, such as nitrates, sulphates, organic chemicals, metals, soil or dust particles, and allergens. Studies on their effect on male fertility have found that PM2.5 particles can have a detrimental impact, increasing the number of spermatozoa with altered head morphology and cytoplasmic droplets, and decreasing sperm concentration and motility.
Other agents that can affect sperm quality include chemicals to which we are regularly exposed. Recent studies have shown that the male reproductive organs are among the primary targets of environmental chemicals, leading to infertility. Consequently, research has linked the exposure of pregnant women to natural or man-made chemicals that mimic, block, or interfere with endocrine system hormones to low sperm concentration in their offspring. These substances are known as endocrine disruptors.
Some of these chemicals that affect male fertility include:
- Dioxins: A group of lipophilic chemicals produced through industrial and natural processes, such as smelting, chlorine bleaching of paper, the production of certain pesticides, and the incineration of biomedical and plastic waste.
- Bisphenols: Bisphenol A is a primary component of plastics and is released into the environment during the production, usage, and disposal of these materials.
- Pesticides and herbicides: especially ethylene dibromide and 1,2-dibromo-3-chloropropane.
- Phthalates: known as phthalic acid diesters, are a group of man-made chemicals that occur universally and are commonly found in products such as toys, pharmaceuticals, cosmetics, building materials, scent enhancers, personal care products, etc. They can be easily absorbed through ingestion, skin contact, or inhaling contaminated air.
How do contaminants affect the sperm quality?
The exact mechanisms by which environmental factors cause male infertility are not known, although much of their effects on the body are understood.
Agents present in polluted air can cause hormonal disruption. Heavy metals such as lead, zinc, copper, and other pollutants in car exhaust have estrogenic, anti-estrogenic, and anti-androgenic effects. These effects can lead to abnormal steroidogenesis and gonadal gametogenesis, thereby altering sperm production. PM2.5 particles accumulate in the reproductive organs through the blood-testicular, epithelial, or placental barriers and can also alter hormone levels, potentially leading to infertility.
Another effect of air pollutants is the increased production of reactive oxygen species, resulting in oxidative stress, lipid peroxidation, and sperm DNA fragmentation, which further contributes to infertility.
Dioxins act as endocrine disruptors by binding to testicular endocrine receptors and altering their function. They are also believed to induce DNA methylation, leading to epigenetic changes in genes that can affect reproductive function, particularly if this exposure occurs before puberty.
Bisphenols exhibit estrogenic, anti-androgenic, and anti-thyroid activities, which may consequently disrupt the hypothalamic-pituitary-gonadal axis and impair reproductive system functions. Increased exposure to BPA causes damage to sperm DNA, mitochondrial dysfunction and degeneration, reduced sperm motility and sperm count, and an increased risk of sperm aneuploidy
Pesticides and herbicides cause direct damage to spermatozoa, alter the function of Sertoli or Leydig cells, and disrupt endocrine function during hormone regulation processes such as synthesis, release, storage, transport, and elimination of hormones; binding of hormones to their receptors; and thyroid function. This can lead to male infertility. Widely used organochlorine pesticides, including DDT and its metabolites, act as endocrine disruptors and may have an anti-androgenic effect, thereby inhibiting the action of testosterone
Phthalates are known for their anti-androgenic activity. They cause a wide range of dysfunctions in male reproductive organs, collectively known as ‘phthalate syndrome’. This syndrome includes decreased anogenital distance, infertility, low sperm count, undescended testes, hypospadias, and various other abnormalities in the reproductive tract
Conclusions
The environment plays a crucial role in male fertility. Adverse environmental factors can lead to a decline in sperm quality, characterized by reduced sperm concentration, motility, and normal sperm morphology, alongside an increase in DNA fragmentation. Decreasing exposure to polluted air and chemicals, and adopting a healthier lifestyle, are necessary steps to mitigate the negative impact of these environmental pollutants on sperm quality and, consequently, on male Fertility
