Egg Bank
Patient first: choose quality, safety and expertise
Profile
Due to our extensive network of oocyte donation centers, we offer a broad range of phenotypes and service choices. Each month, over 100 new donors enroll in our donation programs, enhancing our diversity even further.
At Gametia Biobank we believe that the more demanding we are, the more security we can offer to our collaborating clinics and patients.
This is why our donor selection process is more demanding than the current legal requirements of the European Union and the respective countries of our donation centers.
We continuously expand and improve our donor screening process, following the recommendations of scientific societies such as ESHRE, ASRM, SEF, SIRU, ASEBIR, SIERR and other scientific societies of international relevance. Our scientific team is an active member of most of these societies.

01
Selection process
1.1 – MEDICAL HISTORY
Our selection processes evaluate the reproductive health of donors, previous children, antral follicle count, levels of anti-Müllerian hormone (assessment of ovarian reserve), among other aspects, in order to admit exclusively to our program those candidates who can offer the highest chances of pregnancy to our patients.
A personal and family medical history is carried out, in order to evaluate your medical history and rule out hereditary diseases, according to Spanish Law 9/2014 and RD 412/1996.
An in-person psychological assessment of the donor and her environment is carried out following the recommendations of the Spanish Fertility Society (SEF).
1.2 – ASSESSMENT OF OVARIAN RESERVE
- At Gametia BioBank we only admit candidates for donation whose values significantly exceed those considered normal by the guidelines and recommendations of the main scientific societies such as ESHRE, ASRM, SEF, SIRU, ASEBIR, SIERR, among others.
- AFC (≥20)
- AHM (>3 ng/ml)
1.3 – GENERAL ANALYTICS
- Blood group
- Factor Rh
- Hemogram
- Prothrombin Activity
- TTPA
- Glucose
- Creatinine
- Total cholesterol
- HDL cholesterol
- Triglycerides
- Transaminases (GOT,GPT)
1.4 – INFECTIOUS AND SEXUALLY TRANSMITTED DISEASES
SEROLOGIES
Serological studies are carried out on all donors, both in the selection phase and during treatment and on the day of oocyte retrieval.
* If Anti CMV IgM is positive, a PCR study is performed
VAGINAL DISCHARGE CULTURES AND PCR
Vaginal infections by Chlamydia Trachomatis, Mycoplasma Hominis, Ureaplasma Urealyticum, Neisseria Gonorrhoeae, Trichomonas Vaginalis are ruled out by means of cultures and/or PCR of vaginal discharge, the latter being the most sensitive technique to rule out the presence of any infectious agent, which provides a plus of safety.
The objective is to eliminate pathogenic microorganisms that may cause a pathology in the recipient woman, guaranteeing the safety of the laboratory where in vitro fertilization techniques are performed to avoid contamination that endangers the viability of the technique.
1.5 – CYTOGENETIC STUDIES AND MOLECUAR GENETICS
Only donors with a normal karyotype are accepted. We exclude donors with structural variants (such as duplications, deletions, inversions) of the karyotype, even when not linked to pathological phenotypes. Research indicates that such variants can correlate with poorer outcomes in reproductive processes, prompting their exclusion from our donation programs.
Our donors are evaluated with NextCarrier, an NGS (Next Generation Sequencing) carrier study panel to detect autosomal recessive and X-linked genetic mutations.
In all cases, mutations in the genes responsible for autosomal recessive diseases recommended by the Spanish Fertility Society are studied, which are the most prevalent in the Western European population (cystic fibrosis, spinal muscular atrophy, autosomal recessive deafness, alpha and beta thalassemia, sickle cell anemia), as well as more than 120 mutations associated with X-linked diseases, including fragile X syndrome.
The objective is to significantly reduce the risk of having offspring with any of the aforementioned diseases, included in the recommendations of the Spanish Fertility Society.
Genetic matching is a tool that allows us to compare the genetic information of the donor with that of the male of the recipient couple, with the aim of avoiding the expression of unknown genetic diseases in the offspring. To this end, the study of 2128 genes related to recessive monogenic diseases is carried out.
This analysis is carried out using the latest technology in genetic diagnosis, which is Next Generation Sequencing (NGS).
Among the 2128 genes studied, variants of high prevalence in the Mediterranean area are included.
The results of our donors are compared with the genetic study carried out on the male of the recipient couple, so that we select a suitable donor, so that the donor and the male do not share mutations that could trigger a disease in the offspring.
The ideal genetic matching is one that offers the maximum possibility of reducing the reproductive risk for the diseases included in the carrier study. This is achieved when both individuals providing the gametes have performed the same carrier test.
Many centers conduct carrier tests different from the one we perform on our bank’s donors. In these cases, a donor will be assigned with a negative result (not carrying pathogenic variants) for the genes in which the patient has been found to be a carrier in the report provided to us by the requesting center. Therefore, the genes considered for matching will be those presenting pathogenic and likely pathogenic variants in the test report sent by the requesting center.
(The genetic matching protocol does not eliminate the risk in the offspring of suffering from or being carriers of recessive diseases, even if it is one of the diseases studied. Its objective is to significantly reduce the risks, with the extent of this reduction depending on the disease under study).
At Gametia BioBank, we have a donor DNA bank available. Consequently, in the event of diseases appearing in offspring, we can conduct the necessary studies to assist in diagnosis and treatment in these cases.
1.6 – FACIAL MATCHING SERVICE
The Facial Matching Service is a biometric selection tool for identifying the most suitable donor phenotype for couples. It evaluates over 12,000 biometric distances from each photograph, sorting the results so that the medical team can select the best option in the most efficient way.
FAQs
Ask Us Anything About Our Donation Program
Find the answers to the most frequently asked questions in our centres. If you don’t find your question here, please contact us so that our team can give you a personalized answer.
In each of our locations, gamete donation is regulated by the competent health authorities of each country (Ministry of Health), and our selection and donation criteria are in accordance with these guidelines.
When donors contact our centers, we select those who meet the key criteria to start the donation program, such as age, health status, as well as a satisfactory in-person psychological evaluation.
The age allowed by the health authorities for oocyte donation is between 18 and 34 years old.
Selection criteria are based on phenotypic characteristics, blood type, genetic compatibility ( if a genetic matching is performed).
Anonymous donation is one where personal data regarding the donor’s identity is protected between the recipient and reproduction centers (Spain). In countries like Portugal, donation is “non-anonymous,” and the donor’s identity can be known provided that a series of legal requirements are met.
General information about donors can be known, without including information about their identity. For example, weight, blood type, and some phenotypic characteristics.
Clearly, relevant clinical information can be reported if necessary, at any time, even several years after the donation has been received.
In Spain, the information about the recipient and the donor cannot be disclosed, due to the legal framework of Law 14/2006 in Spain.

02
Genetics
The latest advances in genetics are remarkable, and although there is still much to understand, we have reached a point where existing procedures enable a reduction in the risk of hereditary diseases.
For this reason, we carry out our “Next Carrier Test” to rule out the presence of genetic, pathogenic and likely pathogenic variants related to autosomal recessive and X-linked diseases in oocyte donors.
Our screening significantly reduces the risk of inheritance of the most common autosomal recessive diseases (Cystic Fibrosis, Non-Syndromic Sensorineural Deafness, Beta Thalassemia, Alpha Thalassemia, Sickle Cell Anemia, Spinal Muscular Atrophy, Fragile X Syndrome, Glucose-6-phosphate dehydrogenase deficiency). Nevertheless, to significantly minimize the risk of genetic diseases in offspring, we provide the option of advanced genetic matching. Through this service, we meticulously analyse over 2,000 genes, ensuring comprehensive genetic compatibility.
In the case of very rare genetic diseases present in the patient’s family history, we can develop a specific monogenic search to study the compatible donor, as we keep DNA samples from all our donors.
Scientific studies estimate that most healthy people carry several mutations, which can develop serious genetic disorders in their offspring. In most cases, these genetic mutations show no symptoms and are unknown in the patient’s family history, since for an autosomal recessive genetic disease to develop, it is necessary that the two copies of the gene inherited from an individual are mutated.
If both members of the reproductive couple are carriers of pathogenic variants in the same gene, there is a 25% risk of having a sick child with that specific disorder. If a woman is a carrier of an X-linked disorder, her sons will have a 50% risk of being affected by that specific disorder.
The goal of genetic matching is to compare the presence of mutations with autosomal recessive and X-linked chromosome inheritance in the gametes involved in the assisted reproduction process. Thus, when selecting a donor with genetic matching, the risk of the offspring presenting any of the studied genetic diseases is minimized.This test is recommended in assisted reproduction treatments, but it could also be used in a couple who want to gestate naturally, to ensure that they do not share mutations that could lead to a sick child.
All Gametia Biobank donors are studied through the NEXT CARRIER TEST which evaluates 2128 genes that are related to autosomal recessive and X-linked genetic diseases.
FAQs
Ask Us Anything About Our Donation Program
Find the answer to the most frequently asked questions that arise in reproductive treatments. If you don’t find your question here, please contact us so our team can give you an answer.
- The genetic diseases studied based on recommendations from the Spanish Society of Fertility, being the most common in this region, are:Cystic fibrosis
- Autosomal recessive nonsyndromic sensorineural deafness, type DFNB
- Beta thalassemia
- Alpha thalassemia
- Sickle-cell disease
- Spinal muscular atrophy
- Fragile X-chromosome syndrome
- Glucose-6-phosphate dehydrogenase deficiency
Scientific studies estimate that most healthy people carry several mutations. In most cases, these genetic mutations show no symptoms, since for an autosomal recessive genetic disease to develop, it is necessary for both copies of the gene inherited from an individual to be mutated.
Donors are analysed with genetic tests and thus the status of carrier of autosomal recessive and X-linked genetic mutations is known. This enables the selection of an appropriate donor who does not share genetic mutations with the receiving partner, thus minimizing the risk of the disease manifesting in offspring.
Performing a genetic test such as the “Next Carrier Test” and selecting a donor by doing a genetic matching, provides valuable information to understand the carrier status of genetic mutations that could not be suspected with a medical evaluation or family history. By performing this test and comparing it with the genetic information of the other gamete involved in assisted reproduction therapy, the risk of having children with a genetic disease is minimized.
Because it analyzes ALL pathogenic and likely pathogenic variants in more than 2,100 genes responsible for autosomal recessive diseases as well as more than 120 related to X-linked diseases
03
Services & Methods
SERVICES
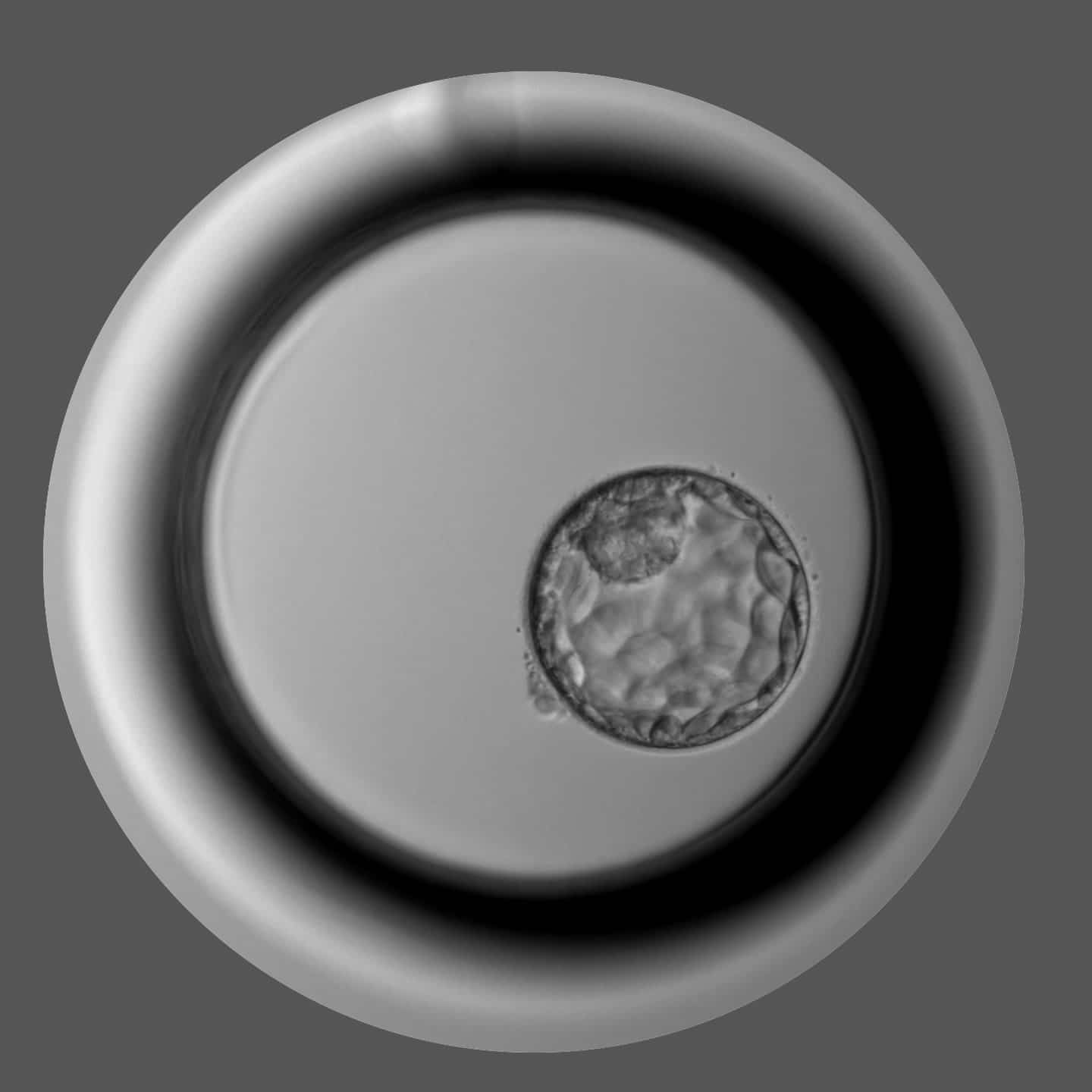
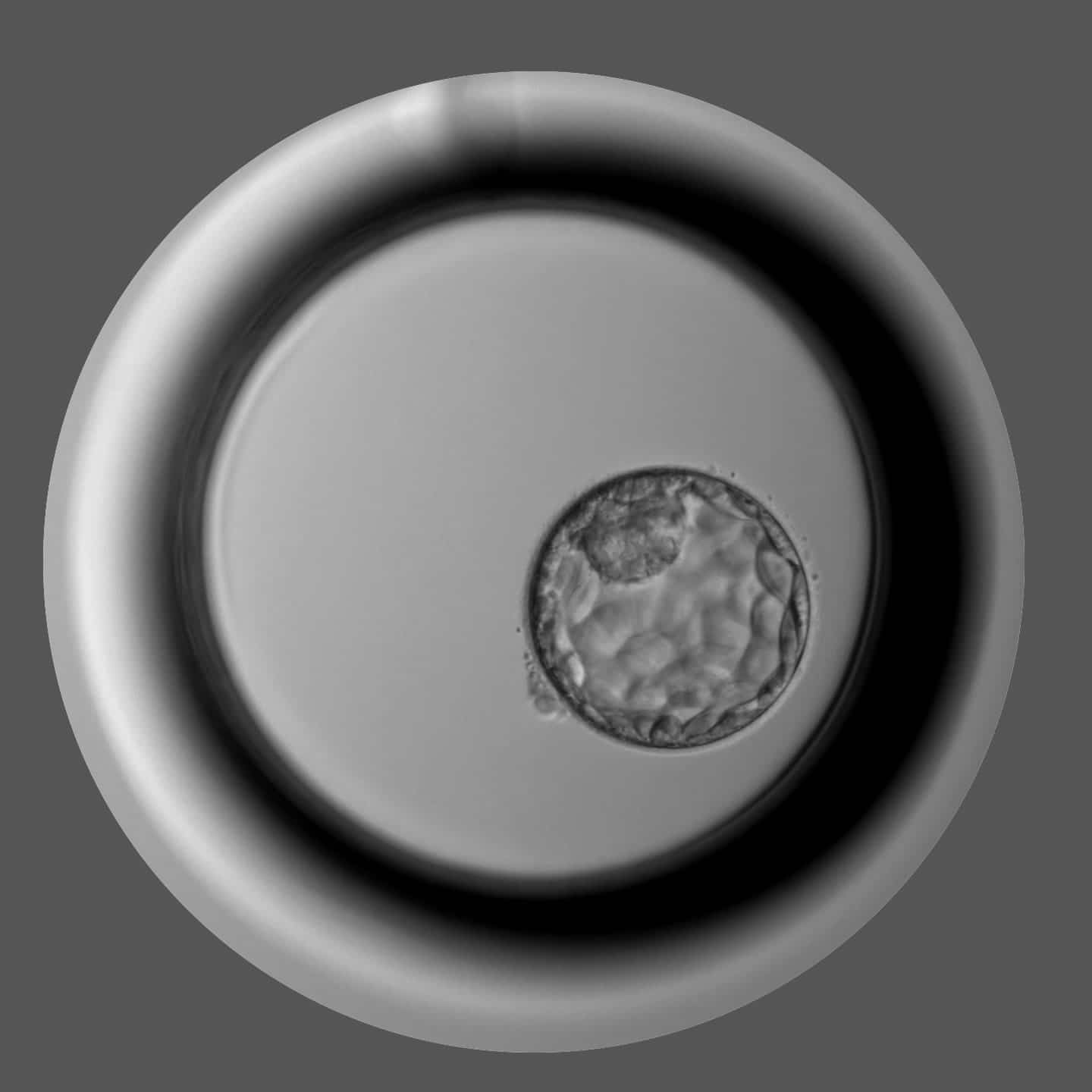
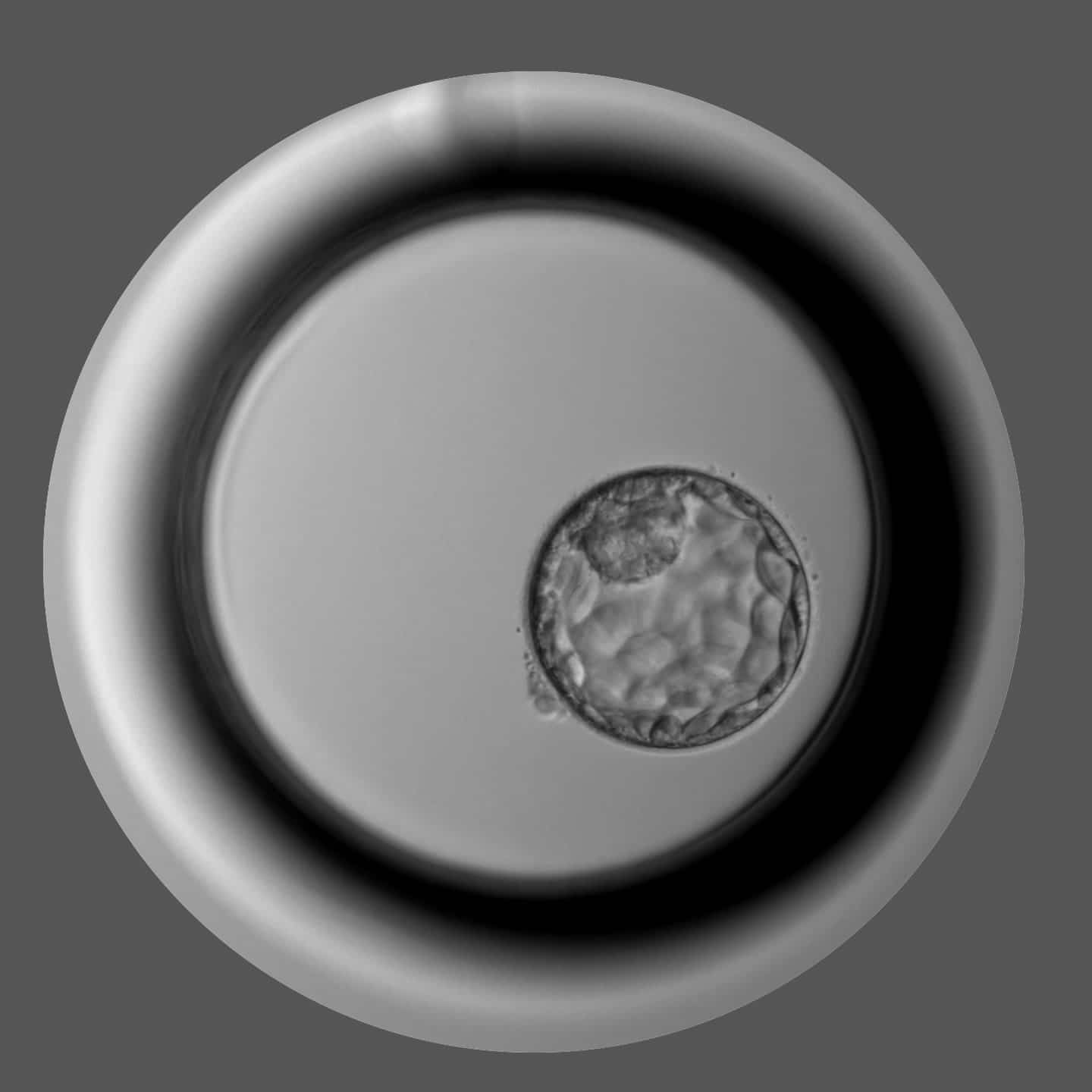
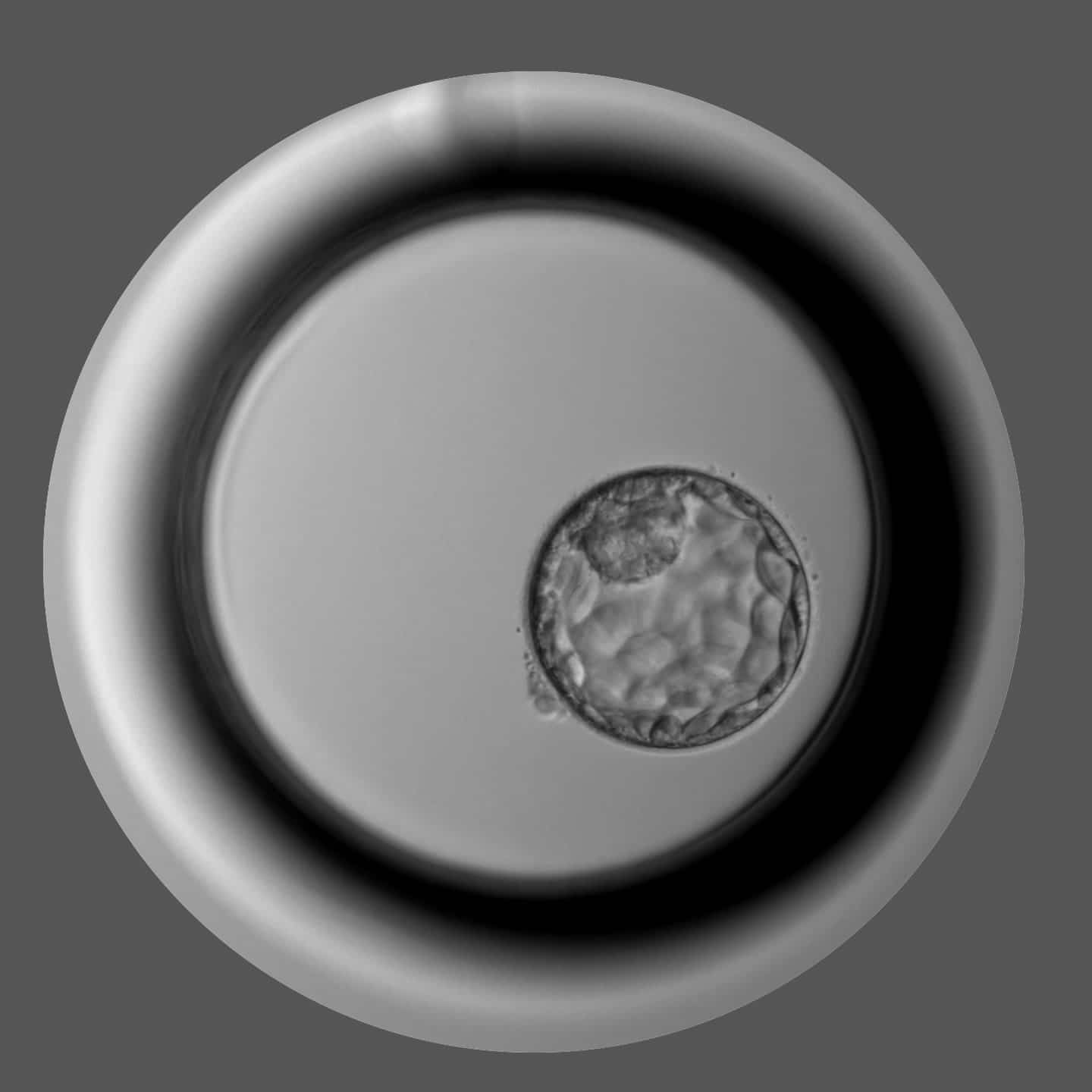
Oocytes: Metaphase II
Gametia can procure oocytes (Metaphase II) obtained from donors following a strict quality control from the donor recruitment to the delivery. Our staff experience, lab technology and support service to our partners result in high clinical results.
Several formats of biological samples are available, depending on the number of oocytes you need: 4,6, 8, 10 or 12 Oocytes, vitrified in Cryotops, two oocytes per device.
(all kinds not only technical)
METHODS
Samples are cryopreserved with Kitazato vitrification media and CryoTop® straws (CE marked), considered as a gold standard in vitrification. Gametia embryologists have a wide experience in vitrification, vitrified over 60.000 oocytes in the past 5 years. The procedures are perfomed daily on a routine basis by the same teams of embryologists, as a result our in-house survival rates are above 92%. PRACTICE AND PRECISION LEAD ALL LABS TO EXCELLENCE. THERE ARE NO SHORTCUTS.
All our devices are CE marked and labelled for an easy access to the relevant information. Each sample is identified with a SEC CODE that follows the latest EU regulations in terms of safety and traceability of tissue samples (EU Directive 2015/565).
As we identify every donation, we store all the history of every single sample and in case of need can give full support.
Each Cryotop is identified with an indelible donor code printing, preventing to mix up straws from different donors and impeding external manipulation of the code, as it cannot be deleted without destroying the label. Additionally, this code makes easier the identification by the receiving Reproduction Center.