Real population, real habits
We have known since childhood about the harmful effects of toxic habits on our health.
Therefore, identifying modifiable lifestyle factors that can predict human fertility and increase a couple’s chances of success with the use of ART has become a major clinical and public health matter.
Cigarette smoking is in fact one of the best-characterized modifiable risk factors for female infertility, numerous epidemiologic studies and a handful of meta-analyses have confirmed that female current smokers have worse reproductive outcomes compared with nonsmokers.
On the other hand, alcohol have historically been the most studied dietary factors in relation to spontaneous fertility, and mixed findings in the existing literature have resulted in a less well-defined understanding of their influence on artificial reproductive technologies success.
Despite this information, it is estimated that almost 50% of women consume alcohol and there are more than 6 million deaths per year related to tobacco use. However, the effect of these substances on the infertile population is still a matter of debate. It is known that the consumption of alcohol or smoking during pregnancy is strictly forbidden, but the time before conception is a grey area where the real harmful effects cannot be fully clarified.
The grey area, how to evaluate such as subjective state?
Most studies evaluating the effects of smoking and alcohol consumption on human fertility are based on a population of couples trying to conceive spontaneously. The reproductive outcomes of couples and women who used these substances were that they took longer to conceive or did not conceive at all. In view of these results, it is assumed that these habits have a negative effect on human fertility.
However, it is difficult to assess the factors that might influence human fertility in such a variable environment as natural conception. Nevertheless, it is crucial to recommend a healthy lifestyle and to try to take the necessary measures to change environmental factors that have a negative effect on general health.
The link between fertility treatments and alcohol or cigarette consumption
Studying patients attending a fertility clinic is more accessible than studying a broad population trying to conceive. There are several scientific publications on the negative effect of alcohol consumption on the outcomes of artificial reproductive therapies, such as a reduction in the number and quality of oocytes and a decrease in implantation rates. However, the influence of smoking habits is still controversial, with some publications finding no negative effect on cycle success rates, but pregnancy rates and obstetric complications are well described in women who smoke.
In order to study this association with better control of bias, Gametia Bank has undertaken a study of the influence of alcohol consumption and smoking in a healthy and fertile population such as egg donors. One of the main strengths of including only donor cycles in this review is the unique opportunity to study many early developmental outcomes, from egg production to maturation and quality, that are almost impossible to observe in naturally conceiving couples.
We design a retrospective comparative cohort study including 507 ovarian stimulation cycles in 2022 and 2023 in our fertility clinics where oocyte donation cycles are performed. We focus the analyses on the effect of alcohol and tobacco use on the number and quality of oocytes after ovarian stimulation. The main outcome was oocyte yield, defined as the percentage of usable oocytes (mature oocytes without intracytoplasmic or extracytoplasmic morphological abnormalities and suitable for ICSI or vitrification) per puncture.
Substance use was divided into four groups: the first group included donors who reported no substance use, the second group included donors who reported only alcohol use (defined by the World Health Organisation as >10 g per day), the third group included donors who reported only smoking, and the fourth and final group included donors who reported the use of both substances. Differences between groups were assessed using Chi-2 for categorical variables and Kruskal-Wallis for continuous variables. Multivariate linear regression was used to adjust for confounders such as BMI, age, gonadotropin dose used, days of stimulation, previous contraceptive use. Statistical significance was set at alpha=0.05 and statistical analysis was performed using Stata version 18.
So, how bad is it?
The results of our study showed that a lower number of total oocytes (23 vs 16 p=<0.001) per cycle, as well as fewer mature oocytes (20 vs 13 p=0.001) and viable oocytes (16.5 vs 12.5 p=<0.001) were observed in the group that consumed alcohol compared to those who did not consume any intoxicant.
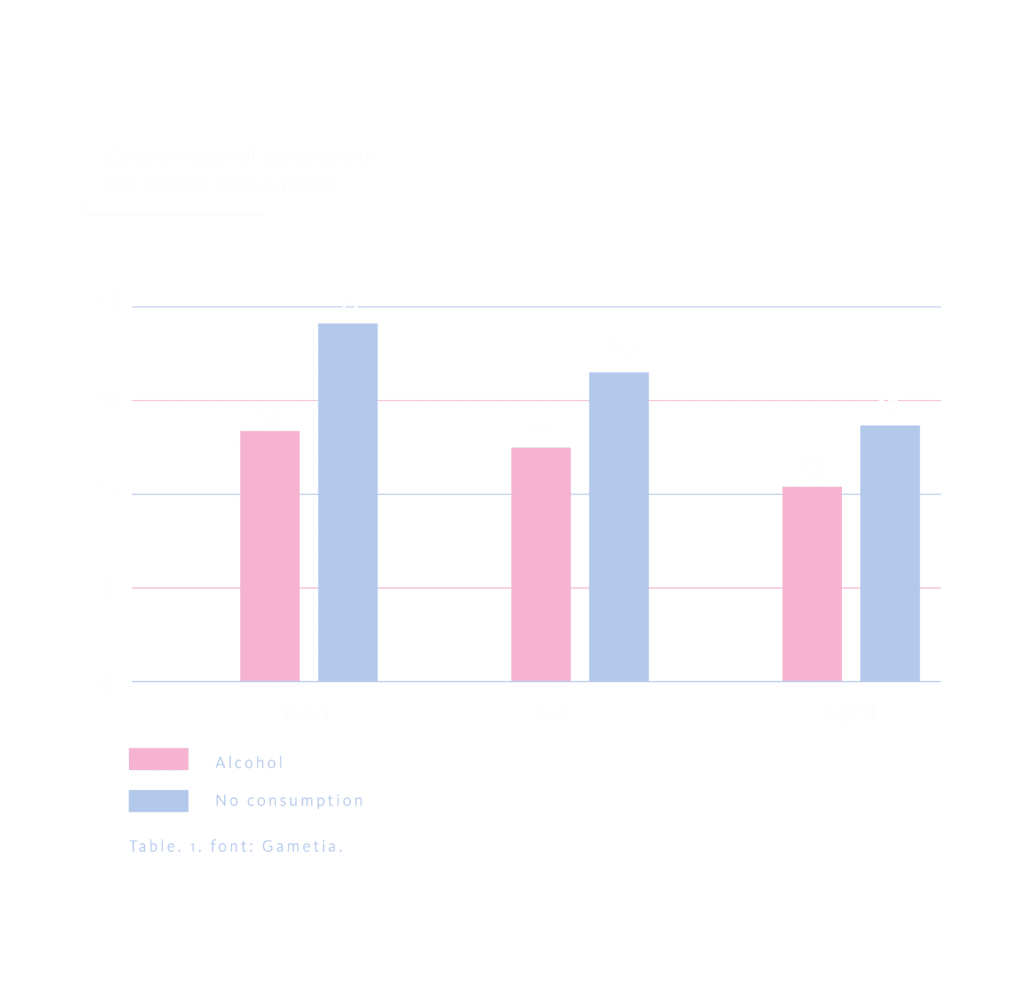
This detrimental effect was more pronounced in the group of alcohol and tobacco users when the oocyte yield was analysed (84.6% vs. 88.9%, p=<0.001).
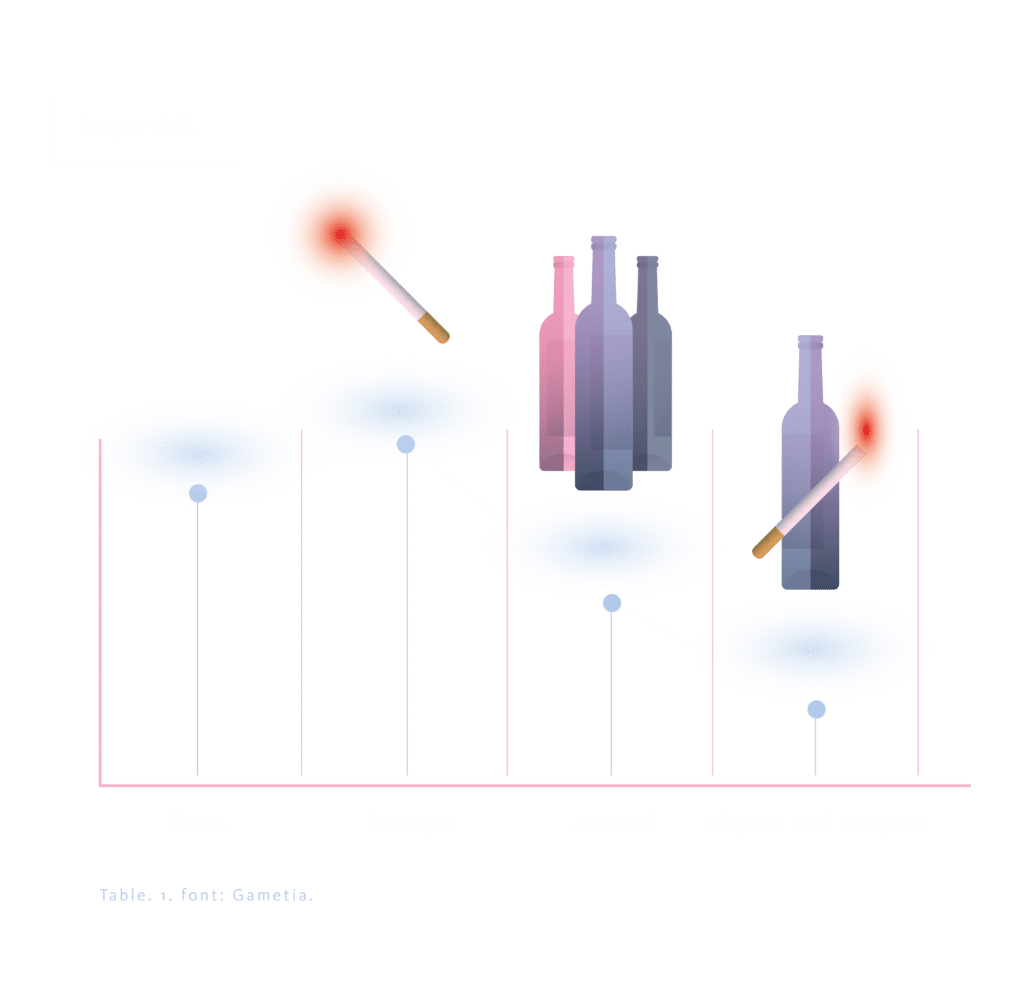
However, when analysing the influence of smoking, no significant differences in oocyte yield were observed between the groups (OR 3.36 95% CI 0.9-7.62 p=0.21). There was no difference in the total dose of gonadotropins used or the number of stimulation days between the groups (p=0.194 and p=0.511).
In conclusion, a negative effect of alcohol consumption on oocyte yield was observed in young, healthy women, and this effect was increased when combined with tobacco use.
In view of this information and the large body of scientific evidence, it is advisable to stop using alcohol and tobacco when trying to conceive and, more importantly, when infertility has been diagnosed and artificial reproductive techniques are required.
Bibliography
- Prieto-Huecas L, Piera-Jordán CÁ, Serrano De La Cruz-Delgado V, Zaragoza-Martí A, García-Velert MB, Tordera-Terrades C, et al. Assessment of Nutritional Status and Its Influence on Ovarian Reserve: A Systematic Review. Nutrients. 2023 May 12;15(10):2280.
- Mínguez-Alarcón L, Chavarro JE, Gaskins AJ. Caffeine, alcohol, smoking, and reproductive outcomes among couples undergoing assisted reproductive technology treatments. Fertility and Sterility. 2018 Sep;110(4):587–92.
- Límites de Consumo de Bajo Riesgo de Alcohol. Actualización del riesgo relacionado con los niveles de consumo de alcohol, el patrón de consumo y el tipo de bebida. Parte 1. Actualización de los límites de consumo de bajo riesgo de alcohol. 2020;(2020).
- Neamtiu IA, Surcel M, Begum TF, Gurzau ES, Berindan-Neagoe I, Braicu C, et al. Specific lifestyle factors and in vitro fertilization outcomes in Romanian women: a pilot study. PeerJ. 2022 Oct 4;10:e14189.
