Fertility preservation has become increasingly important for adults, adolescents, and children due to the growing use of life-saving medical treatments that can affect reproductive potential, particularly through the use of gonadotoxic agents. Two key groups facing this issue are oncology patients and transgender individuals. Many of these patients have only a limited window of opportunity to safeguard their fertility before starting treatments that could compromise their reproductive future. Therefore, it is crucial to offer preservation options that maximize their chances of parenthood later in life. Healthcare providers should engage in open discussions about fertility preservation with patients before initiating any treatments that may impact their ability to have children, ensuring that solutions are tailored to meet each patient’s unique needs.
Current Medical Landscape
While innovations in oncology have led to remarkable improvements in cancer survival rates, treatments such as chemotherapy and radiation, though lifesaving, can have unintended consequences on fertility. These treatments often target rapidly dividing cells, which, unfortunately, include reproductive tissues in both men and women. As a result, cancer survivors may face the harsh reality of infertility following treatment.
Similarly, transgender individuals undergoing hormone therapy or gender-affirming surgeries may experience irreversible changes to their reproductive systems. For many, transitioning is a deeply personal and necessary journey, yet it can present significant challenges regarding future fertility. For instance, testosterone therapy in trans men can suppress ovulation, while oestrogen therapy in trans women can reduce sperm production. Surgical options like oophorectomy or orchiectomy permanently remove reproductive organs, resulting in a loss of fertility.
Studies show that a significant proportion of transgender individuals—around 47%—express a desire to have a child with whom they share a genetic connection. Over half of trans men report wanting children, with approximately 37% wishing to preserve their gametes before undergoing gender-affirming procedures. Among trans women, the percentage of those who wish to have children ranges from 15% to 51%, depending on sexual orientation.
Given these realities, fertility preservation is not merely a medical consideration but a crucial aspect of patient care for those facing treatments that may compromise their ability to have biological children. The timing of this conversation is critical. Healthcare providers must ensure that discussions about fertility preservation occur early, before the initiation of treatments that could affect reproductive potential. Unfortunately, these discussions do not always take place, often due to time constraints, a focus on immediate medical concerns, or a lack of awareness among both patients and providers. However, the emotional and psychological impact of infertility can be profound, making it essential to offer comprehensive, patient-centred care that includes discussions about fertility options.
Techniques in Fertility Preservation
Several fertility preservation techniques enable patients to safeguard their reproductive potential before undergoing treatments that may threaten it. Key advancements include:
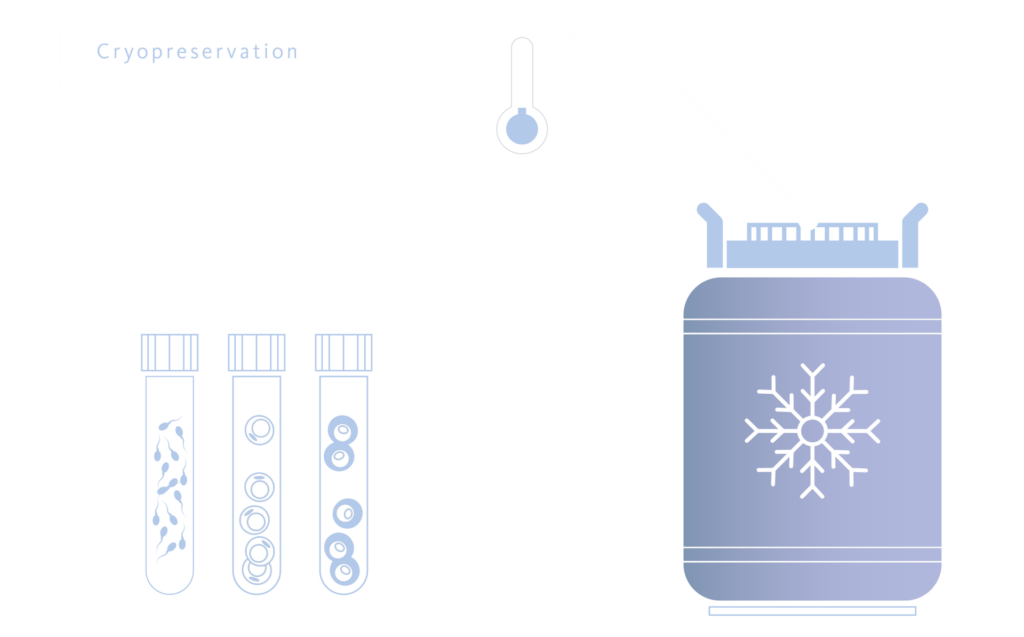
Cryopreservation of Sperm and Oocytes
Vitrification is the most commonly used and effective method for women who have the time to undergo the process before treatment. This technique has greatly improved the survival rates of thawed oocytes and embryos, making it a highly reliable option for fertility preservation. While the process requires ovarian stimulation followed by embryo transfer, some trans men may have already initiated testosterone therapy before undergoing ovarian stimulation. However, studies indicate that testosterone exposure for over a year does not significantly affect the distribution of ovarian follicles. Furthermore, research has shown no significant difference in oocyte yield between trans men on continuous hormone therapy and cisgender women. Given its success rates, vitrification remains a valuable option for fertility preservation.
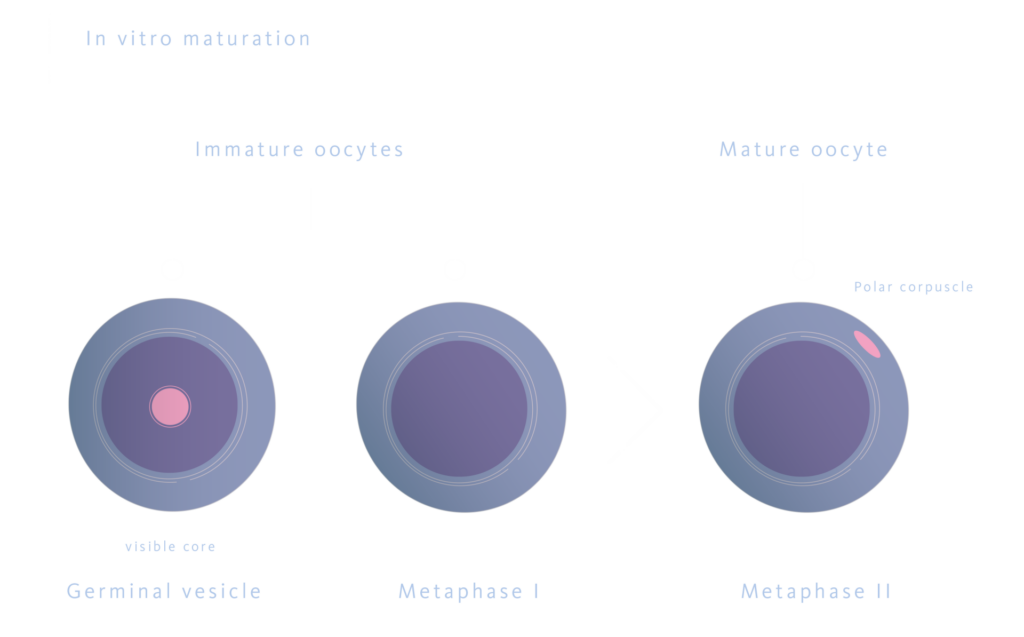
In Vitro Maturation (IVM)
This technique involves the maturation of immature oocytes retrieved from oophorectomy. However, research highlights significant challenges with this approach. Low maturation rates and the overall efficacy of IVM, combined with lower pregnancy rates and a higher risk of pregnancy loss, make it clear that IVM should not be considered the sole method for fertility preservation in trans men.
Sperm Freezing
Whether from ejaculated sperm or surgically retrieved sperm (via TESE), this is a well-established technique with consistently favourable outcomes. The success of pregnancy using cryopreserved sperm largely depends on the sperm’s quality and the type of assisted reproductive technology (ART) employed. High-quality, abundant sperm can be used for intrauterine insemination (IUI), while sperm of lower quality or limited quantity is typically reserved for in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI). However, these techniques are only viable once an individual has reached sexual maturity.
Cryopreservation of Ovarian and Testicular Tissue
Ovarian Tissue Cryopreservation (OTC) is one of the few fertility preservation options available for prepubertal girls and post-pubertal adolescents who are unable to delay gonadotoxic treatments. During this procedure, approximately 50% of the ovarian cortex is surgically removed, dissected, and cryopreserved for future use. The tissue can be preserved using either slow freezing or vitrification techniques. Once thawed, ovarian slices may be transplanted either orthotopically or heterotopically. Orthotopic transplantation (to sites such as the broad ligament or ovarian medulla) offers the possibility of spontaneous conception, while heterotopic transplantation requires the use of assisted reproductive techniques. Currently, OTC is widely recognized as an effective method for preserving female fertility, due to its success in restoring ovarian function and fertility. Recent studies indicate that reimplantation of ovarian tissue into the pelvic cavity restores ovarian function in 85% to 95% of adult recipients, with overall live birth rates ranging from 18.2% to 43.3%.
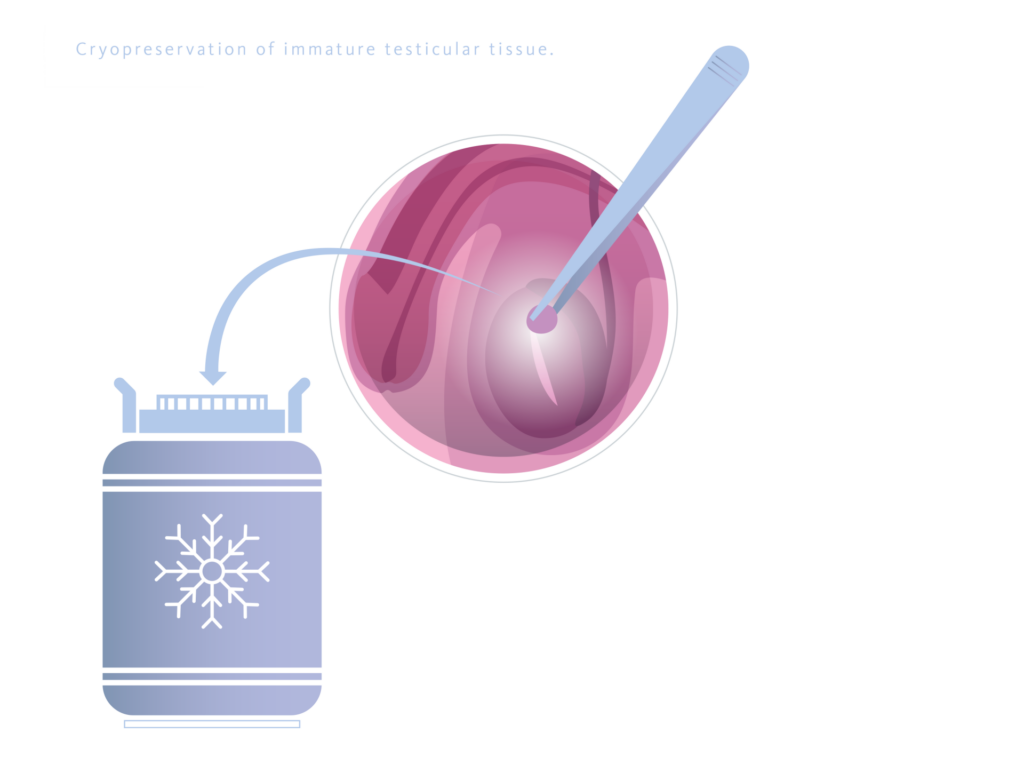
Cryopreservation of Immature Testicular Tissue (ITT)
This is currently the only available option for fertility preservation in prepubertal males who have not yet begun spermatogenesis. This process involves surgically removing small fragments of immature testicular tissue for cryopreservation. Although still experimental, significant advancements are required before testicular tissue cryopreservation becomes a standard clinical practice. The main advantage of ITT grafting is that it preserves testicular stem cells in their natural niche. Additionally, methods have been developed to store these cells in suspension, offering alternative avenues for their future use. Surveys show that many parents are open to this experimental technique, hopeful that advances in reproductive technology will enable fertility restoration when their children reach adulthood.
Ethical and Legal Challenges
Fertility preservation is accompanied by significant ethical dilemmas. In paediatric cases, obtaining informed consent can be particularly challenging. Parents or guardians often make decisions on behalf of minors, raising concerns about the child’s autonomy and their right to make reproductive choices later in life. This situation is further complicated by the fact that children and adolescents may not fully understand the long-term implications of fertility preservation, making it difficult to ensure that their future reproductive rights are adequately protected.
For transgender individuals, issues surrounding gender identity and the desire for biological parenthood add further complexity. These cases require a sensitive approach that respects the patient’s reproductive rights while also considering the medical and technical aspects of their transition. For example, healthcare providers must navigate the delicate balance between supporting a patient’s gender transition and preserving their fertility options. This often involves pausing hormone treatments or planning surgical procedures in a way that maximizes the chances of future biological parenthood.
From a legal standpoint, the preservation of gametes and embryos presents questions of ownership and future use. In some instances, it is essential to establish clear legal agreements regarding the disposition of these materials, particularly in situations involving death or changes in the patient’s circumstances. Legal considerations also extend to the rights of donors and the potential offspring, ensuring that all parties’ interests are protected. Additionally, the evolving landscape of reproductive technology and the varying laws across different jurisdictions can create further legal complexities that must be carefully navigated.
Moreover, ethical considerations also encompass the equitable access to fertility preservation services. Socioeconomic factors, insurance coverage, and geographic location can all influence a patient’s ability to access these services. Ensuring that all patients, regardless of their background, have the opportunity to preserve their fertility is a critical ethical issue that healthcare providers and policymakers must address.
Future Perspectives
Ongoing research in fertility preservation is continuously pushing the boundaries of what is possible. Organoids—miniature, functional organ models derived from stem cells—offer the potential to revolutionize the creation of functional reproductive tissue. These organoids can mimic the structure and function of actual reproductive organs, providing a promising avenue for restoring fertility in patients who have lost reproductive function due to disease or treatment. Additionally, gene analysis and gene editing technologies could potentially prevent, or repair damage caused by aggressive treatments. These technologies hold the promise of correcting genetic defects or enhancing the resilience of reproductive cells to withstand gonadotoxic therapies. However, significant challenges, including ethical considerations, off-target effects, and long-term safety, must be addressed before these methods can be integrated into clinical practice.
Advances in in vitro oocyte maturation and enhanced techniques for preserving testicular and ovarian tissue in paediatric patients also show great promise. These innovations could significantly expand fertility options for populations currently facing limited solutions.
To develop an effective and efficient fertility preservation program, collaboration across various medical and biological disciplines is crucial. This effort should focus on increasing awareness among healthcare professionals and patients about the available options and the importance of early intervention. Educational initiatives and training programs can help ensure that healthcare providers are well-equipped to discuss fertility preservation with their patients. Additionally, addressing and eliminating barriers to accessing fertility preservation services, such as cost, insurance coverage, and geographic availability, is essential to ensure equitable access for all patients.
From a legal standpoint, the preservation of gametes and embryos raises important questions regarding ownership and long-term use. In some instances, it may be necessary to establish clear legal agreements concerning their future use, particularly in cases involving death or changes in the patient’s circumstances.
Conclusion
Fertility preservation is becoming an increasingly critical topic in paediatric and adolescent healthcare, particularly as many malignant diseases are now curable with modern treatments. Innovations in this field are reshaping reproductive medicine, offering renewed hope to oncology and transgender patients at risk of fertility loss.
For healthcare professionals, staying informed about these advancements and understanding their ethical and legal implications is essential for providing comprehensive, personalized care.
The future of fertility preservation appears promising, with emerging technologies poised to expand options for those wishing to maintain their ability to have biological children. However, as these opportunities evolve, healthcare providers must remain vigilant in addressing the ethical and legal challenges, ensuring that fertility preservation decisions are made with full patient comprehension and respect for their rights.
References
- Chen, L., Dong, Z., & Chen, X. (2023). Fertility preservation in pediatric healthcare: a review. Frontiers in endocrinology, 14, 1147898. https://doi.org/10.3389/fendo.2023.1147898
- Lierman, S., Tolpe, A., De Croo, I., De Gheselle, S., Defreyne, J., Baetens, M., Dheedene, A., Colman, R., Menten, B., T’Sjoen, G., De Sutter, P., & Tilleman, K. (2021). Low feasibility of in vitro matured oocytes originating from cumulus complexes found during ovarian tissue preparation at the moment of gender confirmation surgery and during testosterone treatment for fertility preservation in transgender men. Fertility and sterility, 116(4), 1068–1076. https://doi.org/10.1016/j.fertnstert.2021.03.009
- Mattawanon, N., Spencer, J. B., Schirmer, D. A., 3rd, & Tangpricha, V. (2018). Fertility preservation options in transgender people: A review. Reviews in endocrine & metabolic disorders, 19(3), 231–242. https://doi.org/10.1007/s11154-018-9462-3
- Slonim, M., Peate, M., Merigan, K., Lantsberg, D., Anderson, R. A., Stern, K., Gook, D., & Jayasinghe, Y. (2023). Ovarian stimulation and oocyte cryopreservation in females and transgender males aged 18 years or less: a systematic review. Frontiers in endocrinology, 14, 1146476. https://doi.org/10.3389/fendo.2023.1146476