The Spanish National Commission for Assisted Human Reproduction (CNRHA) in March 2021, established a series of recommendations and criteria in relation to the study of reproductive cell donors, in order to establish guidelines that will improve the quality and safety of donations and guarantee the homogeneity of cryopreserved samples.
In Gametia, with the aim of increasing the safety of patients and donors, validation periods of 180 days for male gamete donations are required to corroborate the serological status. The quarantine period can be reduced to 3 months if after that time PCR tests for Hepatitis B and C, HIV and syphilis serology, and they are negative.
Donor seminal samples must be cryopreserved and stored until they can be used in patients. In this cryopreservation process, substances called cryoprotectants are added, which act by protecting sperm from damage that they could suffer when frozen in liquid Nitrogen (N2) at temperatures of -196ºC.
These cryoprotectants must be removed before using the sample in an assisted reproduction technique. In the case of the Ready to use and unwashed sperm samples, from GAMETIA BIOBANK we recommend the application of a wash of the sample at the requesting center, once the straw received is thawed, in order to eliminate as much as possible the cryoprotective medium previously used in its freezing.
Cryopreservation to assure maximum sperm quality
At GAMETIA-BIOBANK, the sperm is cryopreserved using two different systems:
“Ready to use” straws
Prior to freezing, the semen sample is subjected to sperm selection using the density gradient method. In this case, the seminal fluid is removed from the sample and those sperm with the best motility are selected before the cryopreservation process. The sperm sample already selected using the gradient technique is added to the cryoprotectant and frozen in liquid N2 by means of a programmable automatic freezer.
Straws “unwashed sperm”
In this case, a cryoprotectant medium is added to the total fresh, untrained sperm sample and subsequently frozen in liquid N2 with the programmable automatic freezer.
In order to ensure and guarantee a minimum seminal quality after thawing, each frozen sample must also have a post-thaw survival test in which the % of surviving spermatozoa with progressive motility is evaluated.
Minimum sperm quality assurance after thawing
The CNRHA, in its March 2021 document, specifies that the minimum quality that seminal samples must meet, after thawing, must be 3 million sperm with progressive motility in the case of “Ready to use” samples and 10 million sperm with progressive motility for “total semen” samples.
In the available scientific literature, there is controversy when it comes to defining the minimum number of progressive motile spermatozoa that is considered adequate to ensure the maximum pregnancy rate in sperm donor artificial insemination.
Liu et al (2021) consider an optimal amount per insemination, ranging from 3 to 10 million progressive motile spermatozoa, since even if more motile sperm are used, better pregnancy rates are not obtained.
Fang et al. (2011) found no significant differences when they performed inseminations with amounts greater than 2 million progressive spermatozoa.
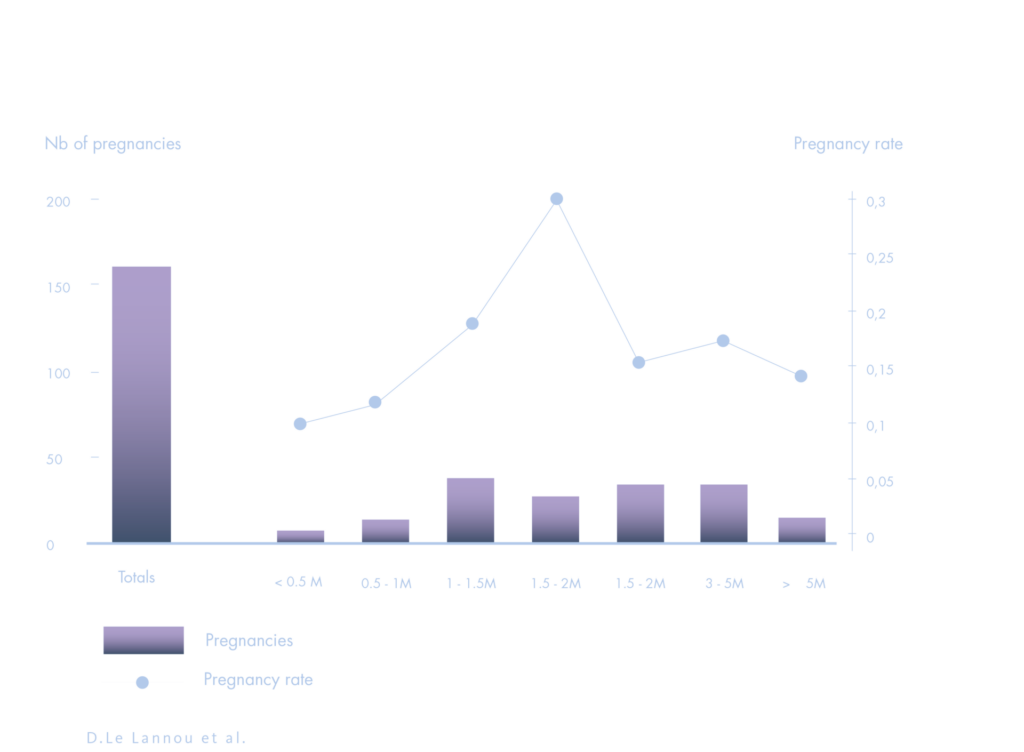
Similarly, Lannou et al. do not find an increase in pregnancy rates when they use more than 1.5 – 2.0 million motile sperm per intrauterine insemination cycle.
Minimum criteria established by GAMETIA BIOBANK
In order to comply with the requirements of the CNRHA report and considering the scientific literature mentioned above, GAMETIA BIOBANK has established minimum criteria in the thawing test to give a sperm donor sample as acceptable.
- The “Ready to use” samples will consist of a test with a minimum of 8 million/ml of progressive motile spermatozoa. Considering that the volume of each straw is 0.5 ml and that only one straw is used per insemination cycle, the minimum number of progressive motile sperm provided will be 4 million per cycle. This number coincides with the minimum amount indicated in the CNRHA report.
- The “total semen” samples will have a minimum test of 10 million/ml of progressive motile spermatozoa. Considering that the volume of each straw is 0.5 ml, the minimum number of progressive motile sperm provided will be 5 million per straw. In this case, and considering that 3 straws are used per insemination cycle, the minimum number of progressive motile sperm provided will be 15 million per cycle. This number exceeds the minimum amount indicated in the CNRHA report.
Sperm quality indicators according to ASEBIR
Once thawed at the petition center, whole semen samples cannot be used until they have been capacitated through the use of some sperm selection technique. At GAMETIA BIOBANK we recommend using density gradients as a selection technique, recommended in turn by the World Health Organization (WHO) in its Manual for the study and processing of semen samples (Who laboratory manual for the examination and processing of human semen) (2021). After applying this technique, only those spermatozoa with progressive motility are selected and, in addition, the seminal plasma and cryoprotectant are eliminated.
The Association for the Study of Reproductive Biology (ASEBIR), in its latest update of quality indicators, establishes that the percentage of recovery of progressive motile sperm (REM) after the use of the density gradient (GD) technique should be greater than 35%. Therefore, if the technique is used properly, after its application to the total semen samples provided by GAMETIA BIOBANK, at least 4.2 million progressive motile spermatozoa should be obtained (15 million minimum progressive motile spermatozoa served in 3 straws x 0.35 (GD effectiveness) = at least 5.25 million progressive motile spermatozoa).
In the literature published to date, it is shown that the pregnancy rate in intrauterine insemination with donor sperm does not vary from the use of 2 million inseminated progressive motile spermatozoa. The seminal samples provided by GAMETIA BIOBANK would be well above these values, 3 million in the case of ready-to-use samples and 5.25 million after the capacitation of the total semen samples.
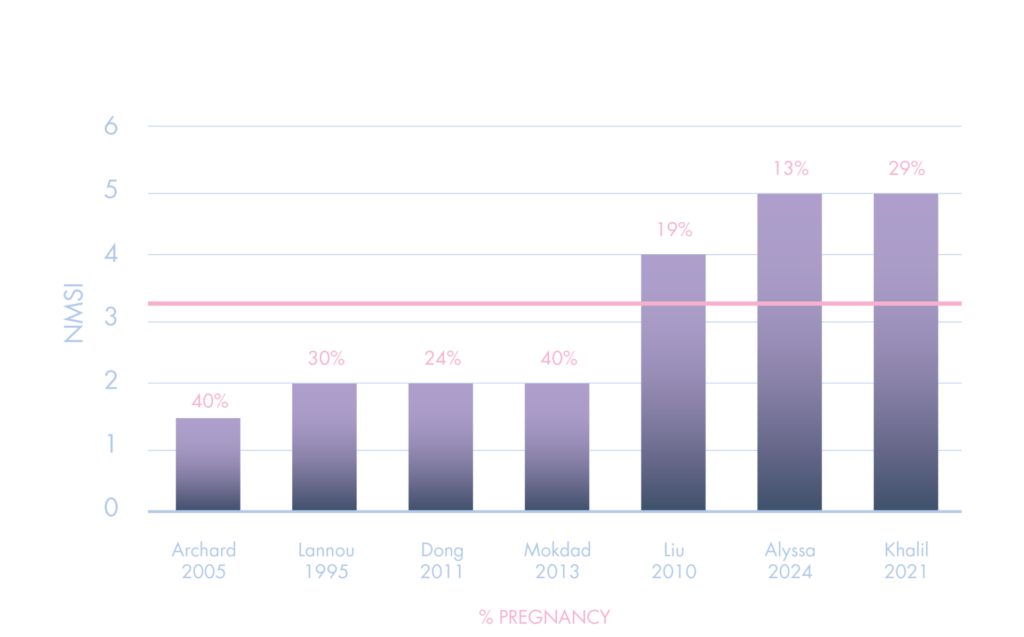
For all the above, based on the available scientific evidence, there is no indication that inseminating with more than two million progressive motile spermatozoa increases the pregnancy rate. Although some biobanks suggest that larger amounts may improve outcomes, this claim lacks strong support in the scientific literature and may be motivated by reasons other than medical criteria. The most important thing is to guarantee the quality and viability of the samples used, always respecting the best clinical practices based on scientific evidence.
References:
- Liu S, Chen Z, Wang H, Yang L, Ma C, Sun L. Prewash and postwash total progressively motile sperm counts have poor predictive value for clinical pregnancy after intrauterine insemination. Int J Gynaecol Obstet. 2021 Jun; 153(3):476-482. doi: 10.1002/ijgo.13447. Epub 2020 Dec 12. PMID: 33119129.
- Fang li Dong, Ying pu Sun, Ying chun Su, Yi hong Guo, Lin li Hu and Fang Wang. Relationship between processed total motile sperm count of husband or donor semen and pregnancy outcome following intrauterine insemination. System Biology in Reproductive Medicine. 2011. 57(5):251-255. doi: 10.3109/19396368.2011.603792.
- Le Lannou D., Gastard E., Guivarch A., Laurent M.C. and Poulain P. Strategies in frozen donor semen procreation. Human Reproduction. 1995. July; Vol 10. Nº7: 1765-1774. doi: https://doi.org/10.1093/oxfordjournals.humrep.a136171.
- WHO laboratory manual for the examination and processing of human semen (6th ed). 2021. World Health Organization.
- National Commission on Assisted Human Reproduction. Activity Report 2018-2021. December 2021.
- Quality Indicators of the Embryology Laboratory.2023. ASEBIR
