The European Society of Human Reproduction recommends a variety of genetic studies at different stages of the reproductive process, the ultimate goal of which is always to minimise the risk of offspring being affected by a genetic disorder. These stages are defined as the Preconception Stage, the Preimplantation Stage and the Prenatal Stage.
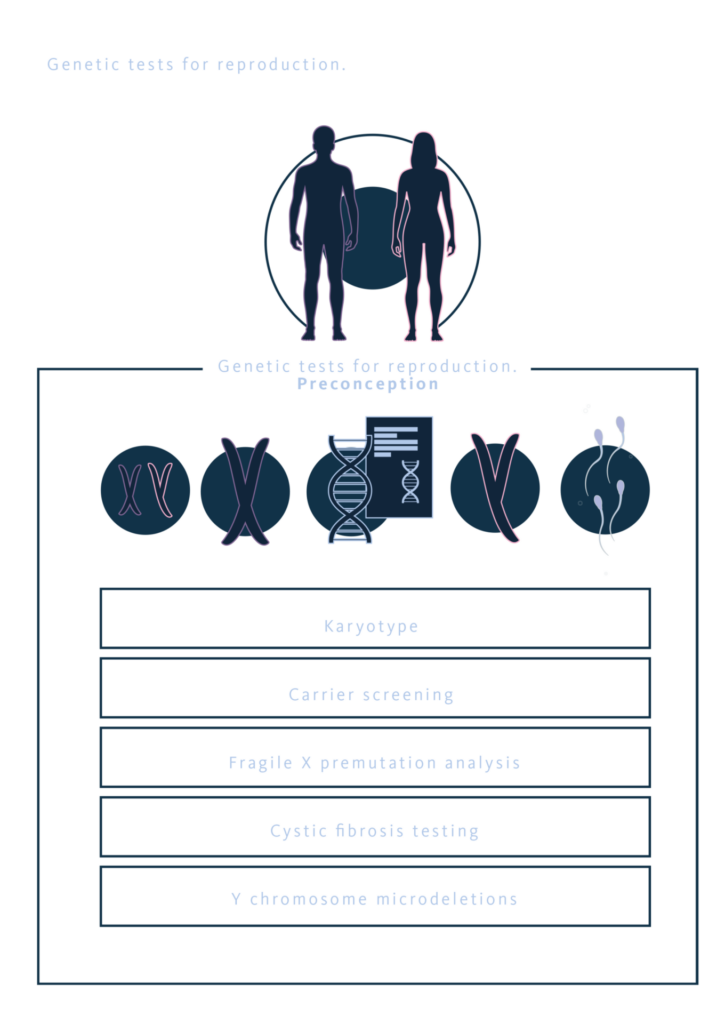
Genetic tests for reproduction: Preconception Stage
From a preventive standpoint, these studies can be initiated even before conception by performing a series of tests to rule out unknown genetic alterations in the parents that could have an impact on their future reproductive health.
Based on a simple peripheral blood sample, these tests include a Karyotype to check for normality, an analysis of Microdeletions on the Y Chromosome and Cystic Fibrosis if there are sperm abnormalities, a study of the FMR1 gene in cases of premature ovarian failure, and a Carrier Study that includes serious and common pathologies in our environment.
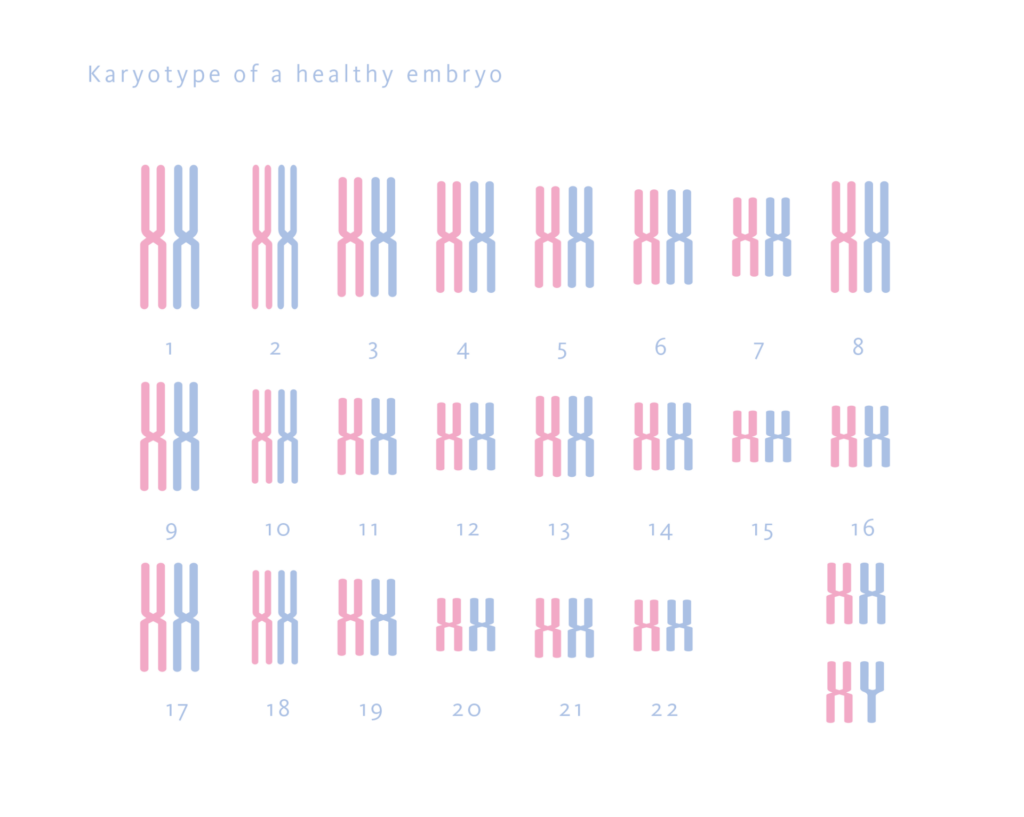
Each of these tests aims to find the cause of possible infertility in an individual. For example, in the case of Karyotype, a common test that analyses the 23 pairs of chromosomes in which our genetic material is distributed, it is possible to detect alterations that do not cause clinical expression in the patient but that can negatively influence their reproductive future by producing incorrect segregation of chromosomes in their offspring and therefore non-viable embryos.
On the other hand, all individuals carry alterations in their genetic material due to the constant mutations that our DNA undergoes from generation to generation. These mutations are sometimes located in genes related to pathologies, such that all individuals can be healthy carriers of between 3 and 6 genetic alterations that will have no consequence on their health, but will affect their offspring when their reproductive partner shares an alteration on the same gene. In these cases, the reproductive risk increases and with it the possibility of having offspring affected by a genetic condition.
Carrier Test is a genetic study that will reveal whether a person is a carrier or non-carrier of a set of diseases. It is therefore essential to consider undergoing this test prior to conception, as the pathologies analysed in this type of test are autosomal recessive or X-linked, and therefore being a healthy carrier of a disorder related to these pathologies is something that we are all unaware of.
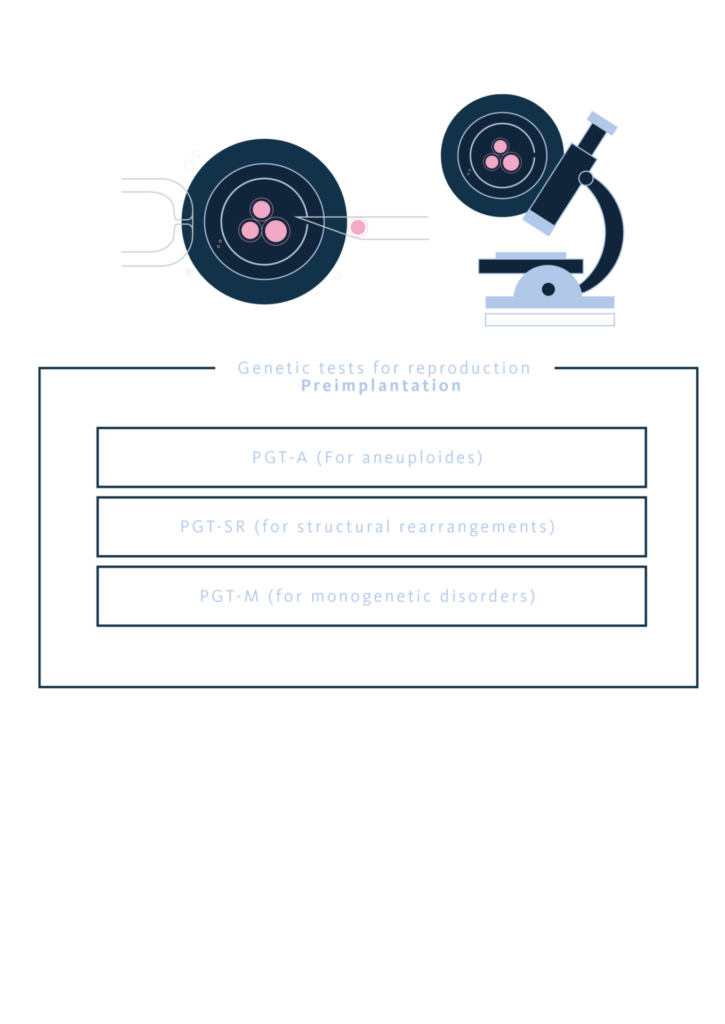
Genetic tests for reproduction: Preimplantation Stage
During the pre-implantation period, genetic tools can also be used to screen the embryos to be transferred or to make an accurate diagnosis related to a genetic disorder. The three most common tests are called PGT-A, PGT-SR and PGT-M.
The PGT-A test or Preimplantation Genetic Testing for Aneuploidy, recommended for women aged 35 and over or for couples with implantation failures or recurrent pregnancy losses, will allow the chromosomal dosage of the embryos to be transferred, ensuring those with the highest chance of resulting in a pregnancy. After in vitro fertilisation, the embryos generated are incubated until day 5. At this point, a biopsy is performed on the outer part of the embryo, the part that will give rise to the placenta during pregnancy, preserving the integrity of the embryo at all times. These cells are analysed using massive sequencing techniques to assess whether each embryo has a normal chromosome dose (Euploid), or an abnormal dose due to loss or gain of genetic material (Aneuploid).
In some embryos, PGT-A testing is likely to result in a Mosaic, reflecting the presence of two different cell lines in the same sample under study. A mosaic can be Low-Grade, when the level of alterations observed in the biopsy is between 30 and 50% of all the cells that make up the sample being studied; or it can be a High-Grade mosaic, when the level of alterations observed in the biopsy is between 50 and 70% of all the cells that make up the sample being studied. If these types of results are obtained, guidance from an embryologist or geneticist is necessary to help the couple choose the best option for achieving a viable pregnancy.
On the other hand, PGT-SR testing or Preimplantation Genetic Testing for Structural Rearrangements, is indicated when one of the parents has a balanced karyotype abnormality. The abnormalities that can be detected with this technique are: translocations, duplications, deletions, insertions and inversions, but always balanced in such a way that there is no loss or gain of genetic material. As these types of alterations are balanced, they do not produce any clinical phenotype in the person who carries them, since the amount of genetic material is normal. However, genetic alterations may occur in their offspring, as the chromosomes will be distributed incorrectly when the meiosis necessary to obtain gametes takes place.
For example, a male with a balanced translocation between chromosomes 2 and 6, that is, part of chromosome 2 has been exchanged with part of chromosome 6, can produce gametes with an erroneous chromosome distribution that will give rise to embryos with trisomy of chromosome 2 or 6, monosomy of chromosome 2 or 6, or embryos with losses or gains of genetic material in the chromosomes involved. In any case, the embryos will be genetically altered and therefore either non-viable or likely to result in individuals with significant genetic disorders.
The PGT-M test or Preimplantation Genetic Testing for Monogenic Diseases, unlike the two previous preimplantation tests, is designed to determine whether embryos generated after a cycle of in vitro fertilisation have a genetic alteration related to the pathology presented by one of the parents in the case of a dominant inherited disease, or by both parents in the case of a recessive inherited disease. This test can only be performed when the disease is sufficiently serious and there are no alternative treatments available.
In the case of a familial disease, the only way to prevent affected offspring is therefore to perform pre-conception embryo selection. Once in vitro fertilisation has been performed and the resulting embryos have been incubated, the PGT-M technique will analyse the DNA of each embryo and identify the healthy embryos. These can then be transferred to the mother’s uterus without risk of developing the disorder. It is a complex process, but completely effective. In order to correctly position the genetic alteration, it is necessary to carry out an Informativeness Study prior to the PGT-M study, which will include samples from the couple and some family members. In this way, the alteration can be detected either directly or indirectly through genetic markers once they have been positioned flanking the family alteration.
It is important to note that some genetic diseases that are candidates for PGT-M testing require in Spain, express authorisation from the National Commission for Assisted Reproduction. These are usually cases in which the genetic alteration is related to a variable form of expression, the disease is related to complex genetics, or the diagnostic criteria are not entirely clear.
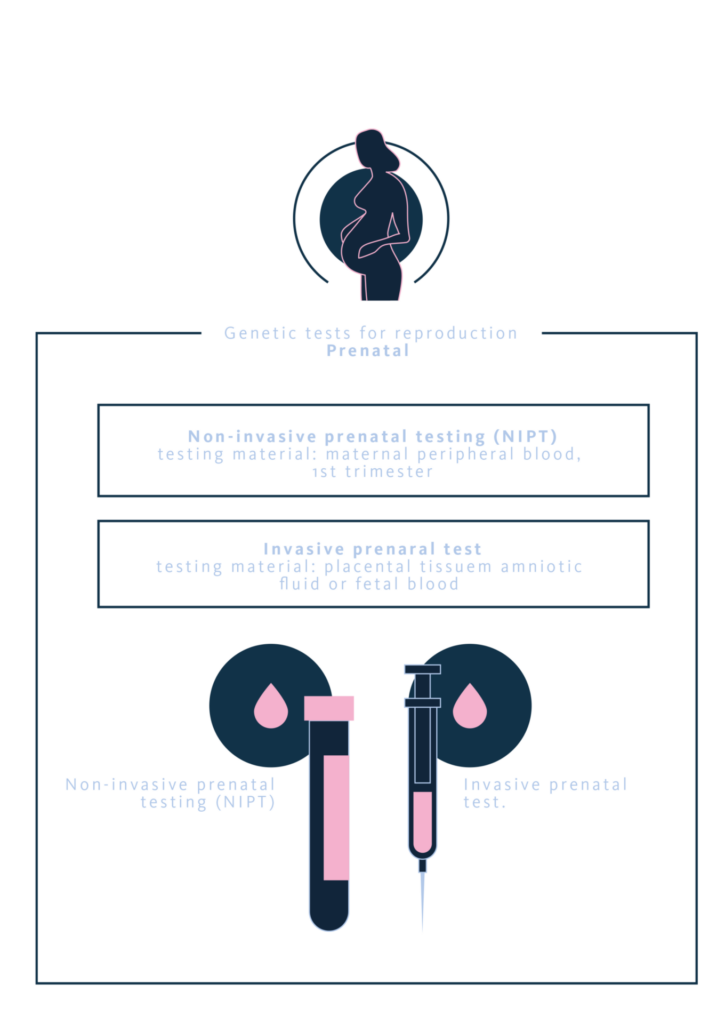
Genetic tests for reproduction: Prenatal Stage
ESHRE recommends two highly useful tests during the prenatal period to determine the genetic status of the embryo. On the one hand, there is the Non-Invasive Prenatal Test (NIPT), a screening test that is performed from the 12th week of gestation onwards and which, using a sample of maternal blood, can detect various abnormalities in the embryo. This test is based on placental DNA circulating in the maternal blood. The technique has a significant false positive rate, as placental cells tend to accumulate genetic abnormalities that are not present in the embryo. However, it is very useful in pregnancies following in vitro fertilisation cycles, where a mosaic embryo or one with partial abnormalities has been transferred, as it allows the couple or pregnant woman to know their reproductive risk as soon as possible. In the event of an abnormal result, an amniocentesis will be necessary to confirm its existence.
On the other hand, Amniocentesis remains the gold standard in invasive prenatal testing, as it directly studies foetal genetic material from epithelial cells present in the amniotic fluid. The test, performed in the 16th week of pregnancy, although uncomfortable for the pregnant woman, provides accurate results about the embryo’s genetics, clearing up any doubts that may arise either after an ultrasound scan, due to the mother’s age, or due to a high risk detected in the first trimester of pregnancy.
Thanks to amniocentesis testing, not only can chromosomal studies be performed on the foetus, but also molecular studies involving panels of genes related to an abnormal ultrasound observation.
Other invasive tests that can be performed once the pregnancy is advanced are Chorionic Villus Sampling, where placental genetic material is accessed between weeks 12 and 13 to detect genetic abnormalities; and a Foetal Blood Test, which is uncommon and only recommended in certain situations, as it is performed after the 18th week of pregnancy and involves a higher risk than amniocentesis. It is only used when other tests have not yielded conclusive results.
There are numerous genetic tests available to professionals and patients, tests that have become indispensable tools at different stages of people’s reproductive lives. All of them require the advice of experienced healthcare professionals.
References
Aynaci et al. 2025: Chromosomal abnormalities in couples with recurrent pregnancy loss: a 16-year cross-sectional study of 4030 cases from Turkey. DOI: 10.5144/0256-4947.2025.154
Chen et al. 2025: Retrospective study on NIPT or NIPT plus combined with ultrasound in screening fetal chromosomal abnormalities. DOI: 10.1038/s41598-025-97230-w
CNRHA 2025: Comisión Nacional de Reproducción Humana Asistida – Ministerio de Sanidad – Gobierno de España.
Dal Molin et al. 2025: Live birth and other reproductive outcomes of mosaic and euploid embryos: a systematic review and meta-analysis. DOI: 10.1007/s10815-025-03575-6
ESHRE 2025: Genetic test for reproduction – Explained
Ethics Committee of the American Society for Reproductive Medicine, 2024: Use of preimplantation genetic testing for monogenic adult-onset conditions: an Ethics Committee opinión. DOI: 10.1016/j.fertnstert.2024.05.165
Lensen et al. 2025: From innovation to practice: evaluating the evidence for preimplantation genetic testing for aneuploidy. DOI: 10.1016/j.fertnstert.2025.05.152
Meng et al. 2025: The efficacy of expanded non-invasive prenatal testing (NIPT) in a high-risk twin pregnancies cohort. DOI: 10.1111/aogs.14958
Poulton et al. 2025: Noninvasive prenatal testing: an overview. DOI: 10.18773/austprescr.2025.019
Tian et al. 2024: Preimplantation genetic testing in the current era, a review. DOI: 10.1007/s00404-024-07370-z
Tzela et al. 2024: Factors Influencing the Decision-Making Process for Undergoing Invasive Prenatal Testing. DOI: 10.7759/cureus.58803
Vendrell et al. 2024: Population-based genetic carrier screening. A consensus statement from the Spanish societies: AEGH, AEDP, ASEBIR, SEAGEN, SEF and SEGCD. European Journal of Human Genetics; https://doi.org/10.1038/s41431-024-01751-3
