The Growing Concern
In recent years, growing concerns have emerged regarding the vast amounts of plastic waste generated by human activity and its potential toxic effects on both human and animal health. Microplastics (MPs) and nanoplastics (NPs) (MNP)—tiny plastic particles—pose significant biological risks, much like their larger counterparts. However, their ability to infiltrate the human body and accumulate in organs raises additional concerns.
These microscopic plastic fragments, present in air, water, food, and even personal care products, have been detected in organs such as the brain, placenta, lungs, testicles, liver, and even breast milk. While the environmental impact of plastic pollution has been extensively debated, its effects on human health—particularly reproductive health—are only beginning to come to light, highlighting an urgent need for further investigation.
Ubiquity of Microplastics and Nanoplastics
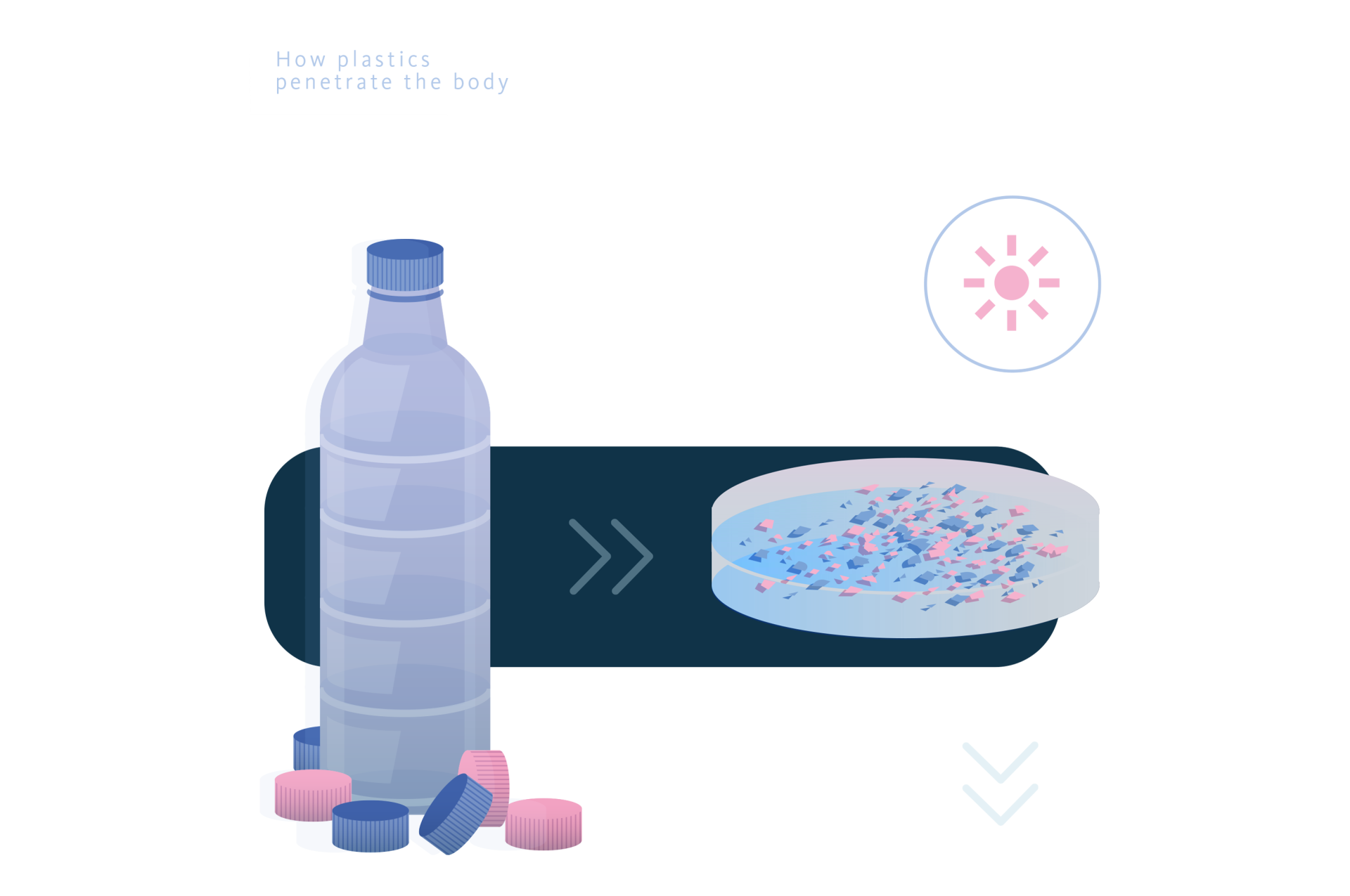
Plastics, synthetic polymers known for their durability and versatility, have revolutionized modern life. However, their widespread use has fostered a throwaway culture, leading to persistent pollution. As larger plastics degrade, they form MPs (≤5 mm) and NPs (<1 μm), which can penetrate biological membranes and accumulate in tissues, including reproductive organs.
MNPs (micro- and nanoplastics) can appear as beads, fibres, or films and are composed of polymers such as polyethylene (PE), polypropylene (PP), polystyrene (PS), and polyvinyl chloride (PVC). They not only exert toxic effects but also carry harmful chemicals, bypassing the body’s detoxification processes and impacting cellular function.
Human Exposure to Micro and Nanoplastics
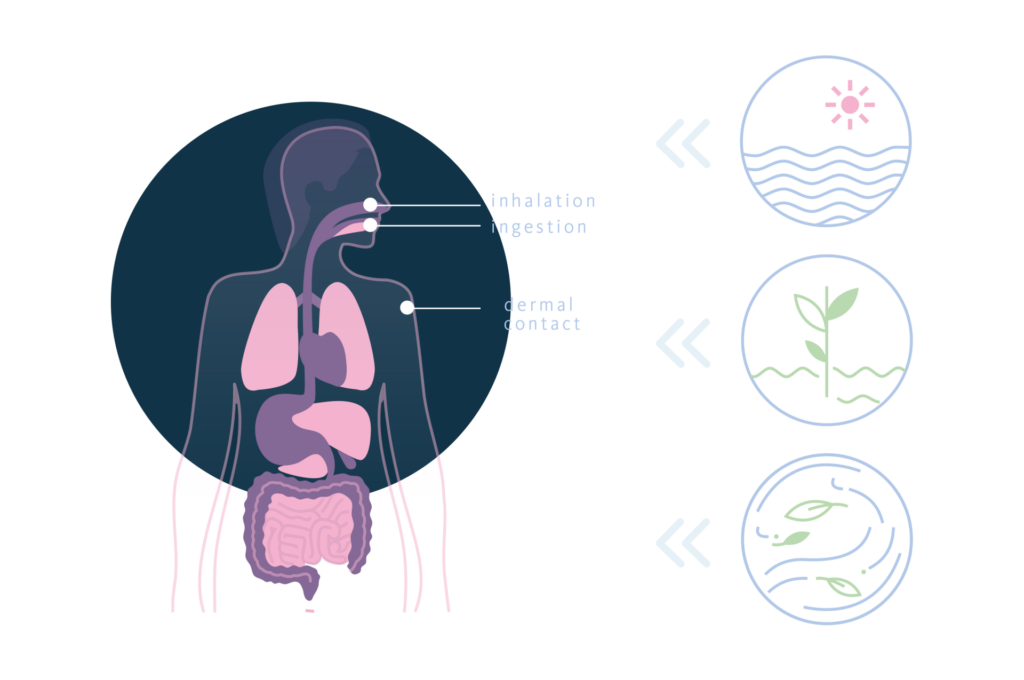
Humans can be exposed to MNPs through three primary pathways: inhalation, ingestion, and dermal contact, with inhalation and ingestion being the most common. While the mechanisms behind this translocation are still under investigation, they are not fully understood. MNPs have been detected in human biological samples, such as blood, urine, sputum, faeces, and breast milk, as well as in organs like the lungs, colon, and spleen. Notably, MNPs have also been identified in the placenta and meconium, indicating potential foetal exposure and raising concerns about developmental toxicity and long-term health risks.
Effects of Micro and Nanoplastics on Reproductive Health
Among the toxic effects exerted by MNPs, the impact on reproduction, including male and female reproductive system as well as embryonal development, is alarming.
The Impact on Male Fertility
Numerous reproductive issues have been reported in male mammals following oral exposure to polystyrene microplastic nanoparticles (PS-MNPs). In rodent models, these particles accumulate in the testes, disrupting the seminiferous epithelium and triggering oxidative stress, mitochondrial dysfunction, and inflammatory responses. They also compromise the blood-testis barrier and hinder Sertoli cell function, leading to a reduction in sperm count, motility, and morphology, as well as lower testosterone and luteinizing hormone levels. MNPs may interfere with pituitary-gonadotropin signalling and overall testicular function. As a result, the reproductive capacity of the exposed rodents is diminished. When the concentration of MNPs in human testes was analysed, polyethylene was found to be the most abundant, and an inverse correlation between testicular weight and MNP concentration was observed. MNP accumulation has also been detected in prostate samples. Moreover, a study revealed elevated MNP concentrations and significant impairment of human semen function. Polystyrene MNPs were found to penetrate and damage sperm cells. Furthermore, the presence of MNPs, along with chemical additives such as phthalates and BPA, can interfere with epigenetic regulation during spermatogenesis, altering gene expression and sperm development. These disruptions may impair fertility and potentially affect future generations. Research shows that phthalates and BPA alter DNA methylation, histone modifications, and RNA expression in sperm, which has been linked to poor sperm quality and fertility issues in humans.

The Impact on Adult Females
In female rodents, oral exposure to polystyrene-MNPs results in accumulation in uterine tissue and ovaries, leading to reduced ovarian weight, altered follicle dynamics, and a decrease in the number of mature follicles. Hormonal changes include lower levels of oestradiol (E2) and anti-Müllerian hormone (AMH), alongside elevated luteinizing hormone (LH), follicle-stimulating hormone (FSH), and testosterone levels. Functional consequences include disrupted oestrous cycles, diminished ovarian reserve, lower embryo implantation rates, and smaller litter sizes. These effects are thought to be driven by MNP-induced oxidative stress, which increases lipid peroxidation, apoptosis, and pro-inflammatory signalling. MNPs have also been identified in the follicular fluid of patients undergoing fertility treatments, showing a significant correlation between MNP concentration and FSH levels, as well as weaker associations with body mass index (BMI), age, and oestradiol, and even reduced oocyte maturation and altered proteomic profiles. Additionally, MNPs, including polyurethane, polypropylene, polystyrene, and polyethylene, have been detected in the human endometrium. Overall, these findings suggest that MNPs may have substantial toxic effects on female reproductive health and fertility, although the full extent of these impacts requires further investigation.
Risks to Pregnancy and Foetal Development
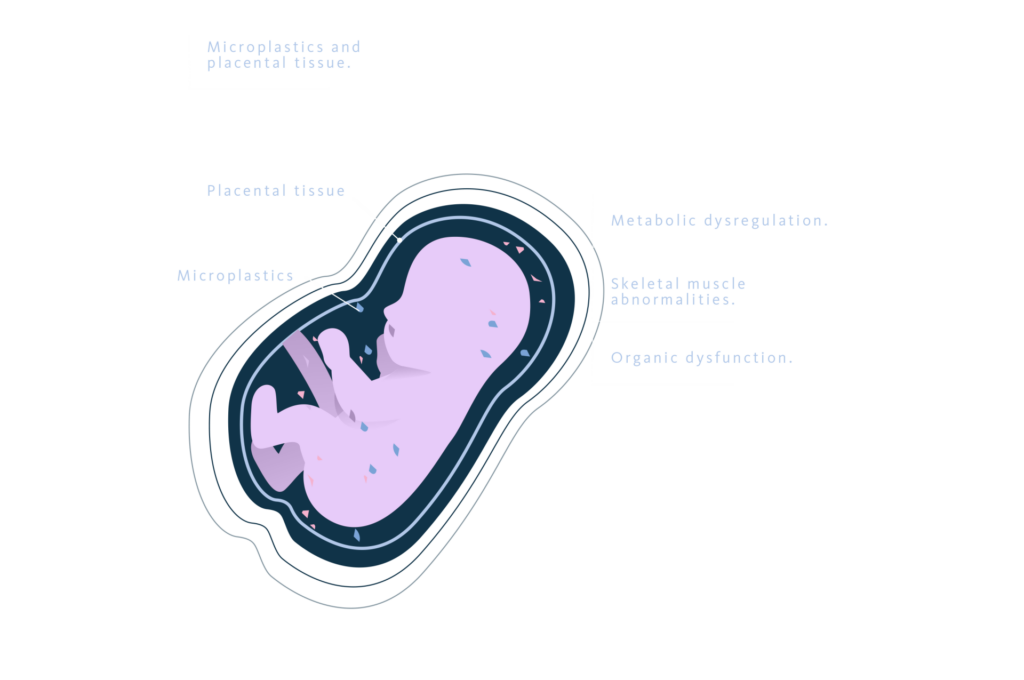
The placenta is essential for nutrient and oxygen exchange between mother and foetus. However, the presence of MNPs in placental tissue raises serious concerns about their impact on foetal development. Studies have linked increased MNP accumulation to placental dysfunction, characterized by altered vascularization and metabolic disturbances that impair foetal growth.
MNPs may also disrupt glucocorticoid signalling, potentially affecting cognitive development and long-term health. Additionally, they have been associated with metabolic dysregulation, skeletal muscle abnormalities, and organ dysfunction. Alarmingly, exposure during pregnancy and breastfeeding may predispose offspring to lifelong health complications, including infertility, cardiovascular disease, and metabolic disorders.
Rodent studies further highlight these risks, showing that higher MNP concentrations during pregnancy correlate with reduced birth weight, length, and head circumference. These findings underscore the urgent need for further research into the long-term consequences of MNP exposure on foetal health and development.
The Need for Action and Further Research
Plastics have become indispensable, yet their unintended consequences for reproductive health cannot be ignored. Despite growing evidence of MNP toxicity, significant gaps remain in our understanding of long-term and transgenerational effects, particularly at low exposure levels. Key priorities moving forward include comprehensive, large-scale epidemiological studies, advancements in detection methods to enhance accuracy in measuring MNP presence in biological samples, and policies to reduce plastic waste, ban harmful additives, and improve waste management. Additionally, educating individuals on plastic-free alternatives and safer consumer choices can help mitigate health risks.
Conclusion
Microplastics and nanoplastics are no longer just an environmental concern—they are a direct threat to human health, particularly reproductive function. From impaired sperm quality to disrupted ovarian function and potential harm to developing foetuses, the evidence underscores an urgent need for further research and action. Reducing plastic exposure is not only essential for our planet but also for the fertility and health of future generations.
References
- Donisi I, Colloca A, Anastasio C, Balestrieri ML, D’Onofrio N. Micro(nano)plastics: an Emerging Burden for Human Health. Int J Biol Sci. 2024;20(14):5779-5792. doi:10.7150/ijbs.99556
- Jaafarzadeh Haghighi Fard N, Mohammadi MJ, Jahedi F. Effects of nano and microplastics on the reproductive system: In vitro and in vivo studies review. Food Chem Toxicol. 2023;178:113938. doi:10.1016/j.fct.2023.113938
- Zurub RE, Cariaco Y, Wade MG, Bainbridge SA. Microplastics exposure: implications for human fertility, pregnancy, and child health. Front Endocrinol (Lausanne). 2024;14:1330396. Doi:10.3389/fendo.2023.133039610.3389/fendo.2023.1330396
