Sexually transmitted diseases (STDs) represent a growing public health concern, as evidenced by published data by the Health Authorities. For instance, the number of syphilis cases surged from 1,010 per 100,000 inhabitants in 1995 to 8,141 in 2022, marking an eight-fold increase. Similar upward trends are observed for other STDs such as gonococcal infection, and chlamydia. The incidence rates are notably higher among men and individuals aged 20-34 years.
While these statistics are concerning, they may only scratch the surface of the issue, with the actual incidence likely being far higher than reported. Therefore, it is essential to establish early detection systems to identify and curb the spread of STDs.
What causes STDs and how are they transmitted?
STDs can be caused by various pathogens, including viruses, bacteria, fungi, and protozoa. For instance, gonorrhoea is caused by the bacterium Neisseria gonorrhoeae; syphilis by Treponema pallidum; chlamydia by Chlamydia trachomatis; genital mycoplasma by Mycoplasma genitalium; trichomoniasis by the flagellated protozoan Trichomonas vaginalis, among others. These diseases are primarily transmitted through unprotected sexual intercourse, vaginal, oral, or anal. Additionally, they can also be transmitted from mother to foetus.
These infections often present with no obvious symptoms, making early detection challenging and increasing the risk of transmission. The lack of symptoms give people a false sense of security, leading to delays in diagnosis and treatment.
Do STDs affect fertility in men and women?
As mentioned earlier, many STDs can be asymptomatic, meaning that a person may have an infection without realising it. However, even if the disease causes no obvious symptoms, fertility and reproductive health is significantly impacted.
How STDs affect fertility in men?
In men, STDs usually cause inflammation of the epididymis, prostate, and testicles, leading to reduced sperm production or blockage of the ducts through which sperm travels during ejaculation.
How STDs affect fertility in women?
In women, STDs usually lead to pelvic inflammatory disease (PID), characterized by inflammation in the pelvic area, potentially damaging the fallopian tubes. This damage can result in blocked tubes, making it challenging for oocytes and sperm to meet, or it would increase the risk of ectopic pregnancy, where an embryo implants outside the uterus. Furthermore, in pregnant women there is an additional risk of transmitting sexually transmitted diseases to the fetus, which can cause significant complications in fetal health, even leading to death.
STD screening in gamete donation programmes
Gamete donors are in the age group in which STD’s are most frequently diagnosed and are therefore of particular interest. In the gamete donation programs perform numerous tests on sperm and egg donors, including STD screening. These tests are performed during the initial evaluation and are repeated every three to six months after donors are accepted into the program. This rigorous testing protocol ensures donors and recipients safety and health, minimising the risk of transmitting infections through donated gametes. By maintaining strict screening and follow-up procedures, these programs help safeguard the integrity of the donation process.
What happens if a donor is found to have an STD?
If a sperm or egg donor tests positive for any of the tested STDs, he or she should be informed immediately so that he or she should avoid risky sexual behaviour and receive appropriate treatment. In general, it is fairly straightforward: most STDs caused by bacteria can be treated with antibiotics, while those of viral origin may require antiviral medication.
After completing the prescribed treatment regimen, the donor will undergo a second round of testing to confirm that the infection has been successfully cleared. This follow-up test is essential to ensure that the infection has been completely eradicated. Only if this subsequent test yields a negative result, indicating no detectable infection, will the donor be considered eligible to participate in the gamete donation program. This protocol ensures the safety and health of both donors and recipients by maintaining the highest standards of medical care and ethical practice in the donation process.
Gamete donation programs as early detectors of STDs
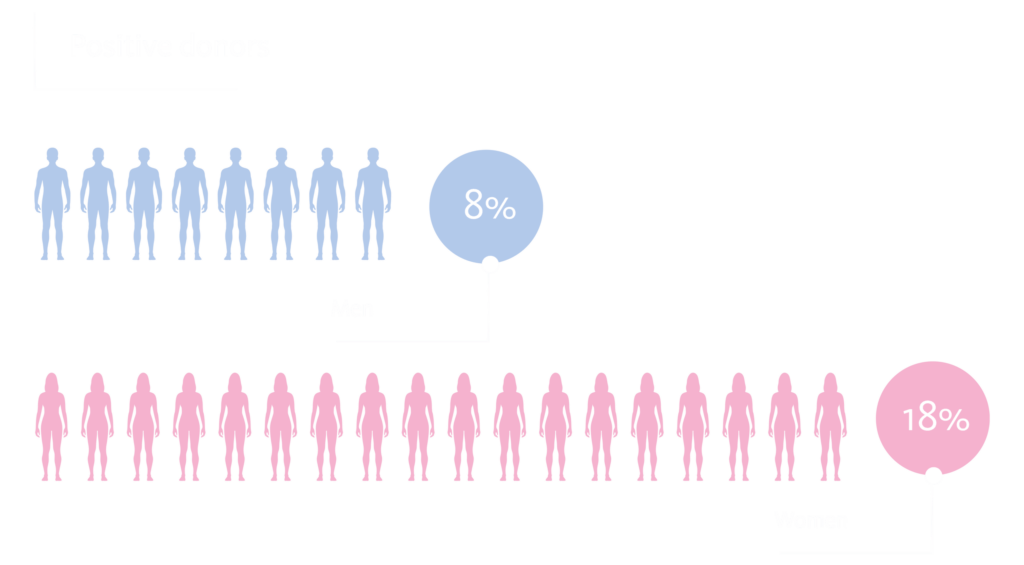
In order to evaluate the role of gamete donation programs as early detection tools for sexually transmitted diseases, the results of the tests performed on egg donors at Next Fertility Murcia and semen donors at GAMETIA Granada during the year 2023 were analysed.
Of the 121 egg donors tested, 22 were found to have one or more of the STDs studied (Neisseria gonorrhoeae, Chlamydia trachomatis, Trichomonas vaginalis, Treponema pallidum and Mycoplasma genitalium). None of them tested positive for hepatitis B or C, nor human immunodeficiency virus (HIV 1 and 2). Chlamydia trachomatis infection was the most frequently detected STD.
As for sperm donors, 226 initial tests were performed on applicants during this period, of which 18 were positive, again with Chlamydia trachomatis infection being the most frequent. One male tested positive for human immunodeficiency virus.
All donors who tested positive were treated and, after repeat testing, their results were negative. This indicates that the treatment protocols were effective and that the gamete donation programs are valuable for both early detection and ensuring the health and safety of all participants in the reproductive process.
Conclusion
The data gathered highlights the significance of routine STD screening in gamete donation programs. By identifying and treating infections early, these programs not only protect the health of donors and recipients but also contribute to the broader public health goal of reducing the prevalence of STDs. Moreover, these results underscore the necessity for continued vigilance and education regarding this matter.
In addition, these findings suggest that gamete donation programs can serve as an important touchpoint for healthcare intervention, offering a unique opportunity to reach individuals who might not otherwise undergo regular health screenings. This proactive approach facilitates timely medical treatment, reduces the risk of spreading infections, and enhances the overall quality of care in reproductive health services. The success of the treatment protocols, as evidenced by the negative follow-up tests, further validates the effectiveness of the healthcare measures implemented by GAMETIA.
Overall, the integration of robust STD screening and treatment protocols within gamete donation programs is instrumental in safeguarding reproductive health, ensuring high standards of care, and supporting public health initiatives aimed at controlling the spread of sexually transmitted infections.
References
- VIGILANCIA EPIDEMIOLÓGICA DE LAS INFECCIONES DE TRANSMISIÓN SEXUAL EN ESPAÑA, 2022. Ministerio de Sanidad. https://www.sanidad.gob.es/ciudadanos/enfLesiones/enfTransmisibles/sida/vigilancia/docs/Informe_Vigilancia_ITS_2022.pdf
